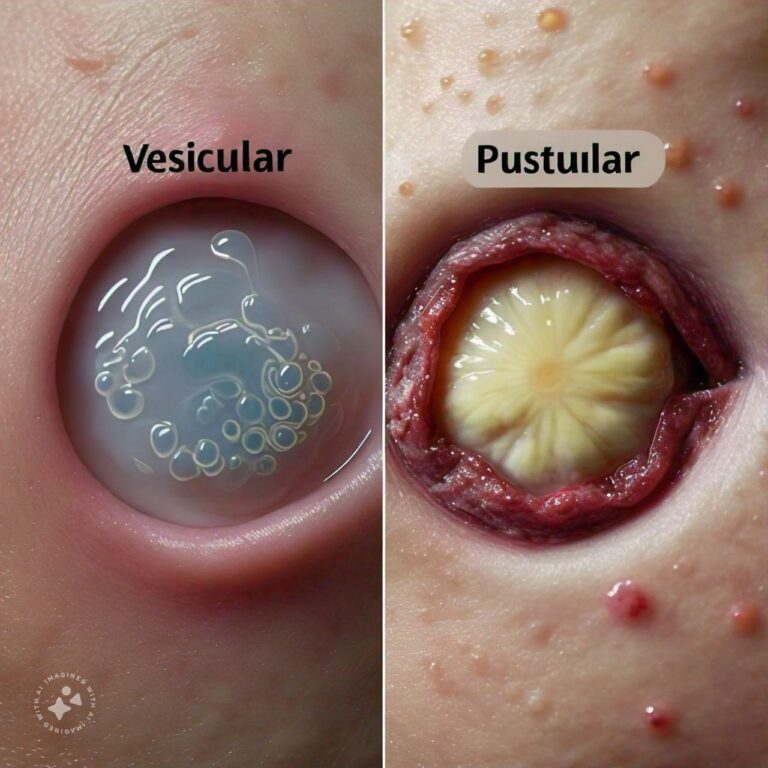
Differences Between Vesicular and Pustular Skin Lesions
Vesicular and pustular skin lesions are two types of abnormal skin growths or blisters that commonly appear in various dermatological conditions. While both are forms of raised skin lesions, they differ in terms of their contents, causes, and the underlying skin conditions they are associated with. Vesicular lesions are characterized by the presence of small, fluid-filled blisters that are usually filled with a clear or straw-colored liquid. These vesicles often occur in clusters and can be caused by a variety of conditions such as viral infections, contact dermatitis, or autoimmune diseases. Vesicular lesions can be extremely itchy and uncomfortable, and if they rupture, they may become painful and prone to infection.
Pustular lesions, on the other hand, are small, elevated skin bumps filled with pus, which is typically a thick, yellowish fluid made up of dead white blood cells, bacteria, and tissue debris. Pustules are commonly associated with bacterial infections, acne, or inflammatory skin conditions like pustular psoriasis. Unlike vesicles, pustules are more closely associated with infection or inflammation and can be painful when touched. While both vesicles and pustules can appear on various parts of the body, their underlying causes and the way they are treated can vary significantly. Understanding the differences between vesicular and pustular skin lesions is crucial for accurate diagnosis and effective treatment.
Vesicular Overview
Vesicular lesions are small, fluid-filled blisters that can appear on the skin due to a variety of causes. Below are five key aspects of vesicular lesions.
1. What are Vesicular Lesions?
Vesicular lesions are small, fluid-filled blisters that appear on the skin. These blisters, known as vesicles, are typically less than 5 millimeters in diameter and are filled with a clear or straw-colored fluid. Vesicles can occur as a result of inflammation, allergic reactions, or infections, and they are often seen in clusters. They can form on any part of the body but are most commonly found on areas that are exposed to irritants or allergens. Vesicular lesions are associated with conditions like herpes simplex virus, chickenpox (varicella), and eczema.
- Fluid-Filled Blisters: Small, raised skin lesions containing clear fluid.
- Common in Infections and Allergies: Often associated with viral infections, eczema, or dermatitis.
2. Causes of Vesicular Lesions
Vesicular lesions can be caused by a wide range of factors, including:
- Viral infections: Conditions like herpes simplex, herpes zoster (shingles), and varicella (chickenpox) cause vesicular eruptions. These infections often produce clusters of vesicles that are painful or itchy.
- Contact dermatitis: Allergic reactions to certain substances, such as poison ivy or nickel, can cause vesicles to form on the skin.
- Autoimmune diseases: Some autoimmune conditions, like pemphigus vulgaris, can cause vesicles to form due to an attack on healthy skin cells by the immune system.
- Viral Infections: Herpes simplex and chickenpox commonly cause vesicular outbreaks.
- Allergic Reactions: Contact with allergens or irritants like poison ivy can lead to vesicle formation.
3. Symptoms of Vesicular Lesions
The symptoms of vesicular lesions include:
- Blistering: The formation of small, fluid-filled blisters that may occur individually or in clusters.
- Itching and irritation: Vesicular lesions are often itchy and uncomfortable, causing the affected person to scratch, which can lead to rupture and secondary infection.
- Pain or burning sensation: In some cases, especially with viral infections like shingles, vesicular lesions can be painful or cause a burning sensation.
- Itchy Blisters: Vesicles are typically itchy and irritating.
- Painful in Some Cases: Certain infections, like shingles, can make vesicles painful.
4. Diagnosis of Vesicular Lesions
Diagnosing vesicular lesions usually involves a physical examination and a review of the patient's medical history. If the cause of the vesicles is unclear, a dermatologist may perform additional tests such as:
- Skin biopsy: A small sample of skin may be taken to analyze the underlying cause of the vesicles.
- Viral culture or PCR: To confirm if a viral infection like herpes or varicella is causing the vesicles.
- Patch testing: This test helps determine if an allergic reaction is responsible for the vesicles, particularly in cases of contact dermatitis.
- Physical Examination: Initial diagnosis is based on visual inspection of the skin.
- Lab Tests: Viral cultures or biopsies may be used to identify the cause of the vesicles.
5. Treatment of Vesicular Lesions
Treatment for vesicular lesions depends on the underlying cause:
- Antiviral medications: If the vesicles are caused by a viral infection like herpes or shingles, antiviral drugs such as acyclovir may be prescribed to reduce symptoms and speed up healing.
- Corticosteroids: For cases involving inflammation, such as contact dermatitis or eczema, topical or oral corticosteroids can help reduce swelling and itching.
- Antihistamines: In cases where itching is severe, antihistamines may be recommended to alleviate discomfort.
- Wound care: Keeping the affected area clean and applying topical antibiotics to prevent secondary bacterial infections.
- Antiviral Drugs: Used to treat viral infections that cause vesicular lesions.
- Topical Steroids: Help reduce inflammation and itching in conditions like eczema or dermatitis.
Pustular Skin Lesions Overview
Pustular lesions are small, elevated bumps filled with pus, commonly associated with infections or inflammatory conditions. Below are five key aspects of pustular lesions.
1. What are Pustular Lesions?
Pustular lesions are small, raised skin bumps filled with pus, a thick fluid composed of dead white blood cells, bacteria, and tissue debris. These lesions are typically white or yellow in appearance and are commonly associated with bacterial infections or inflammatory skin conditions like acne or psoriasis. Pustules can vary in size and may be painful or tender to the touch. Pustular lesions can occur anywhere on the body but are most frequently found on the face, back, and chest, particularly in cases of acne.
- Pus-Filled Lesions: Raised skin bumps filled with pus, a fluid composed of dead cells and bacteria.
- Common in Acne and Infections: Frequently seen in conditions like acne and bacterial infections.
2. Causes of Pustular Lesions
The causes of pustular lesions include:
- Bacterial infections: Conditions like impetigo or folliculitis involve bacterial infections of the skin that result in pustules.
- Acne: Inflammatory acne often leads to the formation of pustules as a result of clogged pores and bacterial overgrowth.
- Pustular psoriasis: A rare form of psoriasis, this condition causes widespread pustular lesions on the skin, often accompanied by redness and swelling.
- Bacterial Infections: Impetigo and folliculitis can result in pustule formation.
- Acne: Pustules are a common feature of inflammatory acne.
3. Symptoms of Pustular Lesions
Common symptoms of pustular lesions include:
- Pus-filled bumps: The hallmark of pustules is their white or yellowish appearance, which indicates the presence of pus.
- Redness and swelling: The area surrounding the pustules is often red and swollen due to inflammation.
- Pain or tenderness: Pustules can be painful, especially when touched or if they are infected.
- Pus-Filled Bumps: Pustules are characterized by white or yellow pus-filled lesions.
- Inflammation: The surrounding skin is often red and swollen.
4. Diagnosis of Pustular Lesions
Diagnosis of pustular lesions typically involves a physical examination by a dermatologist. In some cases, additional tests may be conducted to identify the underlying cause:
- Bacterial culture: A sample of pus may be collected and sent to a lab for bacterial culture to determine the specific organism responsible for the infection.
- Blood tests: In cases of widespread pustular eruptions, blood tests may be necessary to check for underlying systemic conditions.
- Skin biopsy: A small sample of skin may be taken to confirm conditions like pustular psoriasis or other inflammatory disorders.
- Physical Examination: Diagnosis is usually made based on visual inspection.
- Lab Tests: Bacterial cultures and blood tests may be used to identify the cause.
5. Treatment of Pustular Lesions
Treatment for pustular lesions depends on the underlying cause:
- Topical or oral antibiotics: For bacterial infections, antibiotics are often prescribed to eliminate the infection and reduce the formation of pustules.
- Acne treatments: For pustules caused by acne, treatments may include topical retinoids, benzoyl peroxide, or oral medications like isotretinoin.
- Anti-inflammatory drugs: In cases of pustular psoriasis or other inflammatory conditions, anti-inflammatory medications, including corticosteroids, may be used to control symptoms.
- Drainage: In some cases, large or painful pustules may need to be drained by a healthcare professional to reduce discomfort and prevent scarring.
- Antibiotics: Commonly used to treat bacterial infections that cause pustular lesions.
- Anti-Inflammatory Medications: Help control inflammation in conditions like pustular psoriasis.
Differences Between Vesicular and Pustular Skin Lesions
- Contents
- Vesicular: Filled with clear or straw-colored fluid.
- Pustular: Filled with pus, a thick yellowish fluid.
- Cause
- Vesicular: Commonly caused by viral infections, allergic reactions, or autoimmune diseases.
- Pustular: Typically caused by bacterial infections, acne, or inflammatory skin conditions.
- Appearance
- Vesicular: Small, fluid-filled blisters.
- Pustular: Raised, pus-filled lesions that are white or yellow in color.
- Location
- Vesicular: Can appear anywhere on the body but are often associated with conditions like shingles or eczema.
- Pustular: Frequently found on the face, back, and chest, especially in acne cases.
- Symptoms
- Vesicular: Usually itchy and can be painful if they rupture.
- Pustular: Often painful or tender to the touch.
- Infectious vs. Inflammatory
- Vesicular: Often associated with viral infections or allergic reactions.
- Pustular: More likely to be caused by bacterial infections or inflammatory conditions.
- Common Conditions
- Vesicular: Herpes simplex, shingles, contact dermatitis.
- Pustular: Acne, impetigo, pustular psoriasis.
- Treatment
- Vesicular: Antivirals, corticosteroids, and antihistamines are common treatments.
- Pustular: Antibiotics and anti-inflammatory medications are typically used.
- Diagnostic Methods
- Vesicular: May require a viral culture or patch testing.
- Pustular: Often diagnosed with bacterial cultures or skin biopsy.
- Risk of Rupture
- Vesicular: Can rupture easily, leading to secondary infections.
- Pustular: More resistant to rupture but may leave scars if not treated properly.
Conclusion
Vesicular and pustular lesions are two distinct types of skin abnormalities that arise from different causes and require different treatments. Vesicular lesions are small, fluid-filled blisters commonly associated with viral infections, allergic reactions, and autoimmune diseases, while pustular lesions are pus-filled bumps often resulting from bacterial infections, acne, or inflammatory conditions like pustular psoriasis. Understanding the differences between these two types of lesions is critical for proper diagnosis and treatment. Vesicular lesions tend to be itchy and uncomfortable, while pustular lesions are often painful and can leave scars if not treated properly. Both conditions may require medical intervention depending on the severity and underlying cause, but with proper care and treatment, most cases can be managed effectively, allowing the skin to heal without complications.
FAQs
Related Topics
- All
- Animals
- Diseases
- Health
- Money
- Politics
© 2024 OnYelp.com. All rights reserved. Terms and Conditions | Contact Us | About us