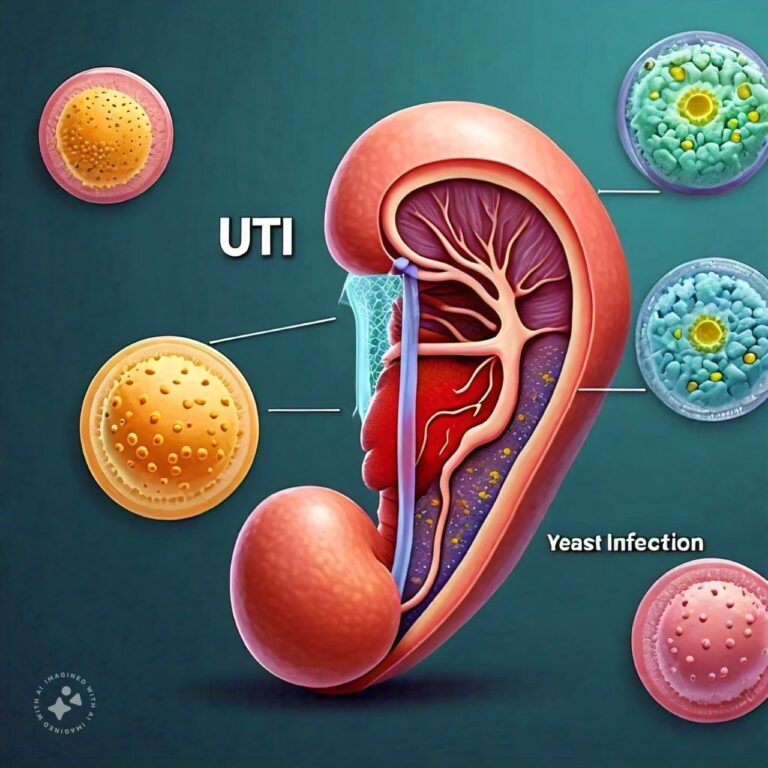
Differences Between UTI and Yeast Infection
Urinary Tract Infections (UTIs) and Yeast Infections are two of the most common health issues that affect women, although men can experience them as well. While they can have similar symptoms, especially discomfort and irritation, they are caused by different pathogens, affect different areas of the body, and require different treatments. A UTI is a bacterial infection that affects the urinary system, which includes the urethra, bladder, ureters, and kidneys. On the other hand, a yeast infection is a fungal infection that occurs when there is an overgrowth of Candida, a type of yeast, typically in the vagina.
Understanding the key differences between UTIs and yeast infections is essential for receiving the right treatment. Misdiagnosing one for the other can lead to ineffective treatments and prolonged discomfort.
UTI Overview
Introduction to UTIs
A Urinary Tract Infection (UTI) is an infection that affects any part of the urinary system, including the urethra, bladder, ureters, and kidneys. Most UTIs involve the lower urinary tract, particularly the bladder and urethra. UTIs are more common in women due to the anatomy of the female urinary system, where the urethra is shorter and closer to the anus, making it easier for bacteria to enter the urinary tract. However, men can also develop UTIs, particularly as they age.
UTIs are caused by bacteria, most commonly Escherichia coli (E. coli), which typically resides in the intestines. When these bacteria enter the urinary tract, they can multiply and cause infection. UTIs can be painful and uncomfortable, but they are usually easily treatable with antibiotics.
Types of UTIs
- Cystitis (Bladder Infection): The most common type of UTI, cystitis occurs when bacteria travel up the urethra into the bladder. It causes symptoms like frequent urination, burning during urination, and pelvic pain. Cystitis is generally not serious but requires treatment to prevent the infection from spreading to the kidneys.
- Urethritis: This type of UTI affects the urethra, causing inflammation and irritation. It can cause burning sensations during urination and discharge. Urethritis can be caused by bacteria from the intestines or sexually transmitted infections (STIs) like gonorrhea or chlamydia.
- Pyelonephritis (Kidney Infection): A more severe form of UTI, pyelonephritis occurs when the infection travels to the kidneys. Symptoms include high fever, chills, nausea, and back or side pain. Kidney infections require prompt medical treatment to prevent damage to the kidneys or the spread of infection to the bloodstream.
Symptoms of a UTI
Common symptoms of a UTI include:
- A strong, persistent urge to urinate.
- A burning sensation during urination.
- Passing small amounts of urine frequently.
- Cloudy or strong-smelling urine.
- Blood in the urine (hematuria), which may appear red, pink, or brownish.
- Pelvic pain, especially in women, often centered around the lower abdomen and pubic area.
- Fever, chills, and flank pain if the infection has spread to the kidneys.
Causes and Risk Factors of UTIs
UTIs are typically caused by bacteria entering the urinary tract. The most common bacteria associated with UTIs is E. coli, which resides in the digestive tract and can sometimes travel to the urethra. The following factors can increase the risk of developing a UTI:
- Sexual Activity: Sexual intercourse can introduce bacteria into the urinary tract, particularly in women.
- Poor Hygiene: Improper wiping after using the bathroom can transfer bacteria from the anus to the urethra.
- Certain Birth Control Methods: Diaphragms and spermicides can increase the risk of UTIs in women.
- Menopause: After menopause, a decrease in estrogen can lead to changes in the urinary tract that make women more susceptible to infections.
- Urinary Catheters: Long-term use of urinary catheters can increase the risk of developing UTIs by introducing bacteria into the urinary tract.
- Kidney Stones or Other Obstructions: Blockages in the urinary tract, such as kidney stones, can prevent proper urine flow and increase the risk of infection.
Diagnosis and Treatment of UTIs
UTIs are typically diagnosed based on symptoms and a urine test. A urinalysis can detect the presence of bacteria, white blood cells, or red blood cells, which indicate an infection. In some cases, a urine culture may be done to identify the specific bacteria causing the infection.
The standard treatment for a UTI is a course of antibiotics, which can clear the infection within a few days. Commonly prescribed antibiotics include trimethoprim/sulfamethoxazole, amoxicillin, ciprofloxacin, and nitrofurantoin. It is essential to complete the full course of antibiotics to prevent the infection from recurring.
Prevention of UTIs
Preventive measures for UTIs include:
- Drinking plenty of water to flush bacteria from the urinary system.
- Urinating after sexual activity to clear any bacteria from the urethra.
- Wiping from front to back after using the toilet to prevent bacteria from spreading from the anus to the urethra.
- Avoiding the use of irritating feminine products, such as douches or scented sprays, which can disrupt the natural balance of bacteria in the genital area.
Yeast Infection Overview
Introduction to Yeast Infections
A yeast infection, also known as candidiasis, occurs when there is an overgrowth of Candida, a type of yeast, in the body. While Candida is naturally present in small amounts in various areas of the body, including the mouth, gut, and vagina, certain factors can cause it to grow out of control and lead to infection. The most common type of yeast infection in women is vaginal candidiasis, but yeast infections can also occur in other areas, such as the mouth (oral thrush) and skin folds.
Yeast infections are not considered sexually transmitted infections (STIs), but sexual activity can sometimes trigger symptoms. They are common in women but can also affect men and children.
Symptoms of a Yeast Infection
Common symptoms of a vaginal yeast infection include:
- Intense itching in the vaginal area.
- Redness and swelling around the vulva.
- A thick, white, odorless discharge that resembles cottage cheese.
- Pain or burning during urination or intercourse.
- Soreness or irritation around the vagina.
Causes and Risk Factors of Yeast Infections
Yeast infections are caused by an overgrowth of Candida albicans, the most common strain of yeast. Several factors can disrupt the natural balance of yeast and bacteria in the body, leading to overgrowth and infection:
- Antibiotics: Taking antibiotics can disrupt the natural balance of bacteria and yeast in the body, allowing Candida to multiply and cause infection.
- Hormonal Changes: Pregnancy, birth control pills, and hormone replacement therapy can all alter the hormonal balance, leading to an increased risk of yeast infections.
- Uncontrolled Diabetes: High blood sugar levels can contribute to yeast overgrowth, as yeast thrives in sugar-rich environments.
- Weakened Immune System: Individuals with weakened immune systems, such as those with HIV/AIDS or undergoing chemotherapy, are at a higher risk of developing yeast infections.
- Damp or Tight Clothing: Wearing tight or damp clothing, such as wet swimsuits or sweaty gym clothes, can create a warm, moist environment that promotes yeast growth.
Diagnosis and Treatment of Yeast Infections
A yeast infection can often be diagnosed based on symptoms and a physical exam. In some cases, a healthcare provider may take a sample of vaginal discharge to confirm the presence of Candida under a microscope.
Yeast infections are typically treated with antifungal medications, which can be applied topically or taken orally. Common treatments include:
- Topical Antifungals: Over-the-counter antifungal creams, ointments, or suppositories, such as clotrimazole, miconazole, or tioconazole, can be applied directly to the affected area.
- Oral Antifungals: Prescription oral antifungal medications, such as fluconazole, are often used to treat more severe or recurrent infections.
For most women, yeast infections are relatively easy to treat and resolve within a few days with antifungal treatment. However, recurrent yeast infections may require longer treatment or a different approach.
Prevention of Yeast Infections
To prevent yeast infections, consider the following tips:
- Maintain good hygiene, but avoid using harsh soaps or douches in the vaginal area.
- Wear loose-fitting, breathable clothing, and change out of wet clothes as soon as possible.
- Manage blood sugar levels if you have diabetes to reduce the risk of yeast overgrowth.
- Avoid prolonged use of antibiotics unless necessary, as they can disrupt the natural balance of bacteria and yeast.
Differences Between UTI and Yeast Infection
- Cause:
- UTI: Caused by bacteria, most commonly E. coli, entering the urinary tract.
- Yeast Infection: Caused by an overgrowth of the fungus Candida, usually in the vaginal area.
- Affected Area:
- UTI: Affects the urinary tract, including the urethra, bladder, and kidneys.
- Yeast Infection: Primarily affects the vaginal area, though yeast infections can also occur in the mouth and skin folds.
- Symptoms:
- UTI: Includes burning during urination, frequent urination, pelvic pain, and sometimes blood in the urine.
- Yeast Infection: Characterized by intense itching, thick white discharge, and vaginal soreness.
- Risk Factors:
- UTI: Common risk factors include sexual activity, poor hygiene, and the use of urinary catheters.
- Yeast Infection: Common risk factors include antibiotic use, hormonal changes, diabetes, and tight clothing.
- Diagnosis:
- UTI: Diagnosed through a urinalysis to detect bacteria or white blood cells in the urine.
- Yeast Infection: Diagnosed through a physical exam and analysis of vaginal discharge under a microscope.
- Treatment:
- UTI: Treated with antibiotics to eliminate the bacterial infection.
- Yeast Infection: Treated with antifungal medications, either over-the-counter or prescription.
- Duration:
- UTI: Symptoms typically improve within a few days of starting antibiotics.
- Yeast Infection: Symptoms usually resolve within a few days of antifungal treatment.
- Prevention:
- UTI: Preventive measures include drinking water, proper hygiene, and urinating after sexual activity.
- Yeast Infection: Prevention includes avoiding douches, wearing breathable clothing, and maintaining good blood sugar control.
- Frequency:
- UTI: Some individuals may experience recurrent UTIs, especially women.
- Yeast Infection: Recurrent yeast infections can occur, particularly in women with hormonal changes or diabetes.
- Contagion:
- UTI: UTIs are not contagious and cannot be passed from person to person.
- Yeast Infection: Yeast infections are not considered sexually transmitted, but sexual activity can sometimes trigger symptoms.
Conclusion
While UTIs and yeast infections can cause similar symptoms, especially discomfort in the genital area, they are distinct conditions caused by different pathogens. UTIs are bacterial infections that affect the urinary tract and require antibiotic treatment, while yeast infections are fungal infections caused by an overgrowth of Candida and are treated with antifungal medications. Understanding the differences between these two common conditions is crucial for proper diagnosis and treatment. Misdiagnosing one for the other can lead to ineffective treatments and prolonged discomfort. If you are experiencing symptoms and are unsure whether it’s a UTI or yeast infection, it’s best to consult a healthcare provider to get the right diagnosis and treatment.
FAQs
Related Topics
- All
- Animals
- Diseases
- Health
- Money
- Politics
© 2024 OnYelp.com. All rights reserved. Terms and Conditions | Contact Us | About us