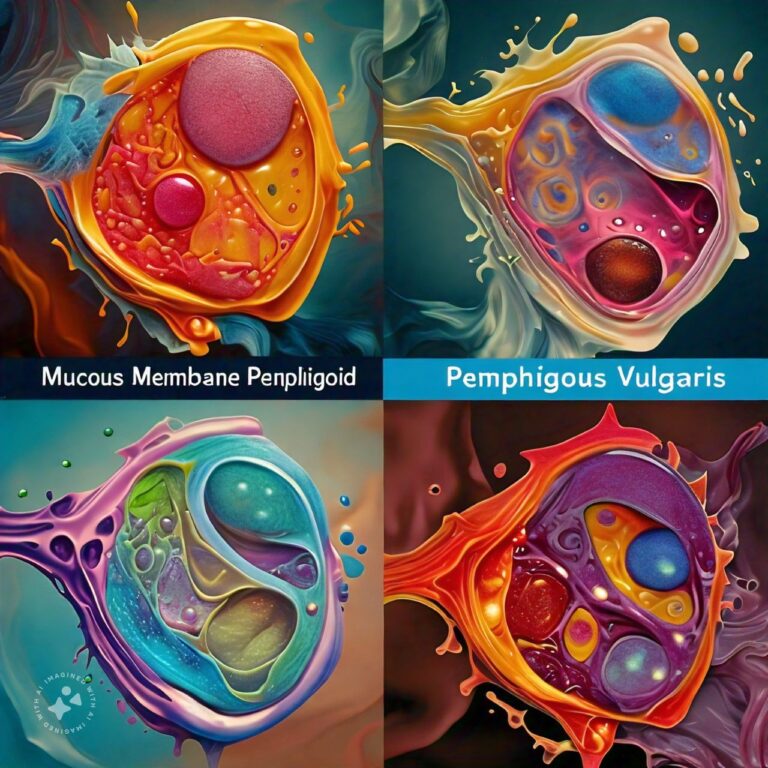
Differences Between Mucous Membrane Pemphigoid and Pemphigus Vulgaris
Mucous Membrane Pemphigoid (MMP) and Pemphigus Vulgaris (PV) are rare autoimmune blistering diseases that primarily affect the skin and mucous membranes. Both conditions arise due to the immune system mistakenly attacking components of the body’s own cells, but they target different structures and manifest in distinct ways. These diseases can significantly impact quality of life and, in some cases, become life-threatening if not managed properly.
In MMP, the immune system targets proteins in the basement membrane zone, the thin layer that anchors the outer layer of skin or mucous membranes to the underlying tissue. This leads to blistering primarily in mucous membranes such as the mouth, eyes, and throat, and occasionally the skin. PV, on the other hand, involves autoantibodies directed against desmogleins, proteins crucial for cell adhesion in the upper layers of the skin. The disruption in cell adhesion causes blisters and erosions on the skin and mucous membranes. Both diseases are chronic and require long-term management, but their treatment strategies differ due to the varied underlying mechanisms.
Mucous Membrane Pemphigoid Overview
1. Pathophysiology of MMP Mucous Membrane Pemphigoid is primarily a result of the immune system’s attack on the components of the basement membrane zone, especially the BP180 and BP230 proteins. These proteins play a critical role in maintaining the adhesion between the outer layers of the epithelium (skin or mucous membranes) and the underlying tissue. When these proteins are targeted by autoantibodies, the bond weakens, resulting in the separation of tissue layers, leading to blister formation. These blisters can heal with scarring, especially in sensitive areas like the eyes, which may lead to severe complications, such as blindness.
2. Clinical Presentation MMP commonly presents as blistering and erosions in mucous membranes, particularly in the mouth, eyes, nose, throat, and genital regions. The oral cavity is most frequently affected, with patients experiencing painful, non-healing ulcers that may interfere with eating and speaking. In ocular MMP, the blisters may cause inflammation and scarring, leading to progressive vision loss. Laryngeal and pharyngeal involvement can result in breathing difficulties due to scarring and narrowing of the airway. Unlike Pemphigus Vulgaris, the skin is only occasionally affected in MMP.
3. Diagnosis of MMP Diagnosing MMP can be challenging due to its varied presentation. It often requires a thorough clinical examination, coupled with a skin or mucous membrane biopsy. The biopsy is essential to look for the specific immune deposits that characterize MMP. Direct immunofluorescence microscopy is typically used to detect these immune complexes, which are found at the basement membrane zone. Blood tests for circulating autoantibodies, such as anti-BP180 and anti-BP230, may also help confirm the diagnosis.
4. Treatment and Management The treatment of MMP is aimed at controlling the immune response to prevent further blister formation and scarring. Corticosteroids are the first line of treatment, often administered topically or systemically depending on the severity of the disease. In more severe cases, immunosuppressive agents such as azathioprine, mycophenolate mofetil, or cyclophosphamide may be required to dampen the immune system’s activity. Early diagnosis and intervention are critical, especially in ocular MMP, to prevent irreversible damage and scarring.
5. Prognosis and Complications The prognosis of MMP depends largely on the extent and location of the disease. If treated early and effectively, many patients can achieve remission. However, complications such as scarring in the eyes (leading to blindness) or airway (leading to respiratory issues) can significantly impact quality of life. Regular monitoring and long-term management are essential to prevent relapses and manage chronic symptoms.
Pemphigus Vulgaris Overview
1. Pathophysiology of PV Pemphigus Vulgaris is an autoimmune disorder characterized by the production of autoantibodies against desmogleins, which are adhesion proteins located in the upper layers of the skin and mucous membranes. Desmogleins are crucial for holding skin cells together. When these proteins are attacked, the adhesion between skin cells breaks down, resulting in intraepidermal blistering. These blisters are fragile and tend to rupture easily, leaving painful erosions.
2. Clinical Presentation PV typically presents with blisters and erosions on both the skin and mucous membranes. The oral cavity is often the first site of involvement, with patients developing painful sores that can interfere with eating and drinking. Skin involvement is widespread, with fragile blisters that rupture easily, leading to large, raw, and painful areas. These areas are prone to secondary infections. Unlike MMP, PV frequently affects the skin in addition to the mucous membranes.
3. Diagnosis of PV The diagnosis of PV involves a combination of clinical presentation, biopsy, and immunological tests. A skin or mucous membrane biopsy showing intraepidermal blistering is often the first step in diagnosis. Direct immunofluorescence is used to detect the presence of autoantibodies against desmogleins in the skin. In addition, blood tests can be used to detect circulating anti-desmoglein antibodies, which are often elevated in PV patients.
4. Treatment and Management The management of PV requires aggressive immunosuppression to halt the immune-mediated destruction of skin cells. Systemic corticosteroids are typically the first line of treatment, often combined with steroid-sparing agents such as rituximab, azathioprine, or mycophenolate mofetil. Because long-term steroid use can have significant side effects, these additional immunosuppressive drugs help reduce steroid dependency. Patients require close monitoring to manage both the disease and the potential side effects of treatment.
5. Prognosis and Complications Without treatment, PV can be fatal, primarily due to infections that develop in the open skin sores. However, with modern immunosuppressive therapies, many patients achieve remission or at least significant improvement. Long-term management is essential to prevent relapses, which are common even in treated patients. The main complications arise from both the disease and its treatment, including infections, adverse effects of immunosuppressive drugs, and, in severe cases, poor healing of skin and mucous membrane lesions.
Differences Between Mucous Membrane Pemphigoid and Pemphigus Vulgaris
- Target Proteins: MMP targets proteins in the basement membrane (BP180 and BP230), while PV targets desmogleins in the upper layers of the skin.
- Blister Location: MMP primarily affects mucous membranes (mouth, eyes, throat), while PV affects both mucous membranes and the skin more extensively.
- Nature of Blisters: MMP blisters are subepidermal and deeper, whereas PV blisters are intraepidermal and more superficial.
- Scarring: MMP often leads to scarring, particularly in sensitive areas like the eyes, while PV generally does not result in scarring.
- Ocular Involvement: MMP frequently affects the eyes, leading to complications like blindness, whereas ocular involvement in PV is rare.
- Severity of Skin Involvement: PV often involves widespread skin blistering, while MMP rarely affects the skin and focuses more on mucous membranes.
- Autoantibodies: MMP is associated with autoantibodies against BP180 and BP230, while PV involves autoantibodies against desmogleins 1 and 3.
- Prognosis: MMP tends to have a more chronic course with complications like scarring, while PV can be life-threatening if untreated but is often manageable with aggressive immunosuppression.
- Treatment Approach: PV often requires more aggressive systemic immunosuppressive therapy due to the extensive skin involvement, while MMP may respond to topical treatments if mucous membranes are the primary site of disease.
- Infectious Risk: PV patients are at higher risk of secondary skin infections due to extensive skin erosions, while MMP patients are less likely to develop such infections due to limited skin involvement.
Conclusion
Mucous Membrane Pemphigoid and Pemphigus Vulgaris are serious autoimmune blistering diseases that, while rare, require careful diagnosis and long-term management. While they share similarities, they differ in the underlying targets of the immune response, clinical presentation, and long-term outcomes. Early diagnosis and treatment are critical in managing both diseases to prevent severe complications such as scarring and infection. With appropriate care, many patients can achieve remission and maintain a good quality of life.
FAQs
Related Topics
- All
- Animals
- Diseases
- Health
- Money
- Politics
© 2024 OnYelp.com. All rights reserved. Terms and Conditions | Contact Us | About us