- Hormone Levels:
- Hypopituitarism: Involves a deficiency in one or more hormones produced by the pituitary gland.
- Hyperpituitarism: Involves excessive production of one or more pituitary hormones.
- Common Cause:
- Hypopituitarism: Often caused by trauma, infection, or tumors that damage the pituitary gland.
- Hyperpituitarism: Usually caused by a pituitary adenoma that increases hormone production.
- Growth Effects:
- Hypopituitarism: Can lead to stunted growth or delayed development in children due to a lack of growth hormone.
- Hyperpituitarism: Causes excessive growth (gigantism or acromegaly) due to overproduction of growth hormone.
- Impact on Metabolism:
- Hypopituitarism: Results in a slower metabolism, often leading to fatigue and weight loss.
- Hyperpituitarism: Can lead to an increased metabolism, rapid weight gain, and high blood pressure.
- Sexual and Reproductive Symptoms:
- Hypopituitarism: Causes reduced libido, infertility, and menstrual irregularities due to low levels of sex hormones.
- Hyperpituitarism: May cause overproduction of prolactin, leading to menstrual changes in women and erectile dysfunction in men.
- Common Hormone Deficiencies/Excess:
- Hypopituitarism: Often involves deficiencies in cortisol, thyroid hormones, growth hormone, and sex hormones.
- Hyperpituitarism: Usually involves excess production of growth hormone, ACTH, or prolactin.
- Diagnosis Tools:
- Hypopituitarism: Diagnosed through hormone deficiency tests and imaging for pituitary damage.
- Hyperpituitarism: Diagnosed through hormone excess tests and imaging to detect adenomas.
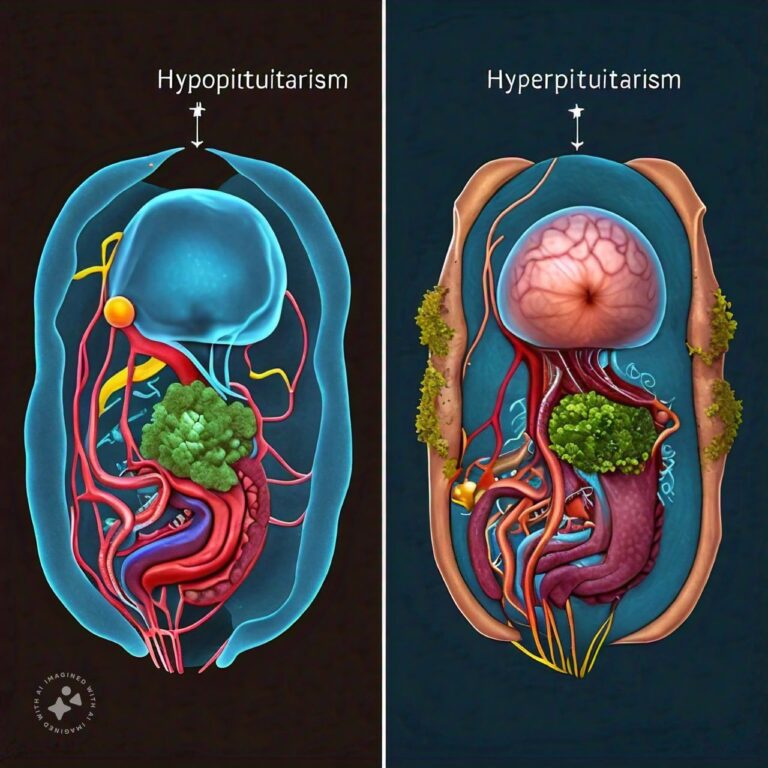
Differences Between Hypopituitarism and Hyperpituitarism
Hypopituitarism and hyperpituitarism are both disorders related to the functioning of the pituitary gland, a small but crucial gland located at the base of the brain. The pituitary gland, often referred to as the “master gland,” controls the release of hormones that regulate many essential body functions, including growth, metabolism, and reproduction. When the pituitary gland doesn’t function properly, it can either underproduce hormones (hypopituitarism) or overproduce hormones (hyperpituitarism), leading to a wide range of health problems.
Hypopituitarism occurs when the pituitary gland is unable to produce enough of one or more hormones, leading to deficiencies that can affect various parts of the body. This condition can be caused by head trauma, tumors, infections, or autoimmune conditions. In contrast, hyperpituitarism happens when the pituitary gland produces an excessive amount of hormones, which can lead to symptoms such as rapid growth, weight gain, or high blood pressure. Both conditions are serious and require medical intervention, but they differ in their underlying causes, symptoms, and treatment approaches.
Hypopituitarism Overview
1. Causes of Hypopituitarism
Hypopituitarism is caused by damage to the pituitary gland or the hypothalamus, the part of the brain that controls the pituitary. This damage can result from a variety of factors, including head injuries, tumors, infections (such as meningitis or tuberculosis), radiation treatment for cancer, or surgery. Autoimmune disorders, where the immune system mistakenly attacks the body’s own tissues, can also lead to hypopituitarism by damaging the pituitary gland.
In some cases, hypopituitarism may be congenital, meaning a person is born with the condition due to genetic mutations that affect pituitary development. It can also develop gradually over time or occur suddenly, such as after a traumatic injury or stroke.
2. Symptoms of Hypopituitarism
The symptoms of hypopituitarism vary depending on which hormones are deficient and how severe the deficiency is. Common symptoms include fatigue, weakness, and weight loss, which are often linked to adrenal insufficiency caused by low cortisol levels. A deficiency in thyroid-stimulating hormone (TSH) may lead to symptoms such as dry skin, cold intolerance, and constipation, while low levels of gonadotropins (LH and FSH) can cause infertility, reduced libido, and irregular menstrual cycles in women.
In children, growth hormone deficiency can result in slowed growth or short stature. In adults, it may cause decreased muscle mass and energy. Additionally, deficiencies in antidiuretic hormone (ADH) can lead to excessive thirst and urination, a condition known as diabetes insipidus.
3. Diagnosis of Hypopituitarism
To diagnose hypopituitarism, doctors typically perform a combination of blood tests to measure hormone levels and determine which hormones are deficient. If a pituitary tumor is suspected, imaging studies such as magnetic resonance imaging (MRI) or computed tomography (CT) scans may be used to assess the size and location of the tumor. In some cases, doctors may use stimulation tests to assess how well the pituitary gland responds to signals from the hypothalamus.
A thorough medical history and physical examination are essential to help identify the underlying cause of hypopituitarism, whether it is related to injury, infection, or a more chronic condition.
4. Treatment for Hypopituitarism
The treatment for hypopituitarism focuses on replacing the deficient hormones and treating the underlying cause of the condition. Hormone replacement therapy is the primary form of treatment and may include cortisol (to replace adrenal hormones), thyroid hormone, growth hormone, and sex hormones (such as estrogen or testosterone). Patients will need lifelong hormone replacement therapy to manage their condition effectively.
If a tumor is causing hypopituitarism, surgery may be necessary to remove it. In some cases, radiation therapy may also be required to shrink the tumor or prevent it from growing further.
5. Prognosis and Management of Hypopituitarism
With proper treatment and hormone replacement, individuals with hypopituitarism can lead relatively normal lives. However, they must be vigilant about managing their condition, as hormone levels need to be carefully monitored and adjusted over time. Regular follow-up appointments with an endocrinologist are essential to ensure that hormone replacement therapy is working effectively and that any underlying issues, such as tumors, are being addressed.
Hyperpituitarism Overview
1. Causes of Hyperpituitarism
Hyperpituitarism occurs when the pituitary gland produces too much of one or more hormones, usually due to the presence of a pituitary adenoma (a benign tumor). These tumors can affect hormone secretion by either producing hormones themselves or by causing the pituitary to release excess hormones. Most pituitary adenomas are non-cancerous, but they can still cause significant health issues.
Other causes of hyperpituitarism include genetic mutations, conditions such as McCune-Albright syndrome, or damage to the hypothalamus, which can lead to excessive stimulation of the pituitary gland.
2. Symptoms of Hyperpituitarism
The symptoms of hyperpituitarism depend on which hormones are being overproduced. For example, if the pituitary produces too much growth hormone, it can lead to a condition called acromegaly in adults or gigantism in children. Both conditions are characterized by abnormal growth of bones and tissues, resulting in enlarged hands, feet, and facial features, or excessive height in children.
Excessive production of adrenocorticotropic hormone (ACTH) can lead to Cushing’s disease, which is characterized by rapid weight gain, high blood pressure, and changes in skin appearance, such as a “moon face” or “buffalo hump.” In women, overproduction of prolactin can result in irregular menstrual cycles or infertility, while men may experience decreased libido and erectile dysfunction.
3. Diagnosis of Hyperpituitarism
Diagnosing hyperpituitarism involves blood tests to measure hormone levels and imaging studies (such as MRI or CT scans) to identify the presence of a pituitary adenoma. If specific symptoms point to excess hormone production, further tests may be performed to determine which hormones are involved and the extent of the excess.
Doctors may also perform a suppression test, where medications are used to see if hormone levels can be reduced, helping to confirm a diagnosis of hyperpituitarism.
4. Treatment for Hyperpituitarism
The treatment for hyperpituitarism often involves surgery to remove the pituitary adenoma, especially if it is causing significant symptoms or hormone imbalances. In cases where surgery is not possible or effective, medications may be used to reduce hormone levels. For example, dopamine agonists can be used to lower prolactin levels, while somatostatin analogs can help reduce growth hormone production.
Radiation therapy may also be an option to shrink the tumor and prevent further hormone production. Long-term management involves regular monitoring of hormone levels to ensure that the condition remains under control.
5. Prognosis and Management of Hyperpituitarism
The prognosis for individuals with hyperpituitarism depends on the cause and severity of the condition. If a pituitary adenoma is successfully removed, patients may see a significant improvement in symptoms. However, some individuals may need long-term medication or hormone therapy to manage their condition. Regular follow-ups with an endocrinologist are crucial for monitoring hormone levels and adjusting treatments as necessary.
Differences Between Hypopituitarism and Hyperpituitarism
- Treatment Approach:
- Hypopituitarism: Treatment primarily involves hormone replacement therapy to supplement the deficient hormones.
- Hyperpituitarism: Treatment often focuses on reducing hormone levels, typically through surgery to remove pituitary adenomas, medications, or radiation therapy.
- Symptoms:
- Hypopituitarism: Symptoms include fatigue, weight loss, cold intolerance, muscle weakness, and infertility due to insufficient hormone production.
- Hyperpituitarism: Symptoms include abnormal growth (gigantism or acromegaly), rapid weight gain, high blood pressure, and skin changes due to excess hormones.
- Long-term Management:
- Hypopituitarism: Involves lifelong hormone replacement and regular monitoring of hormone levels.
- Hyperpituitarism: Requires ongoing monitoring after treatment, especially if surgery or radiation was involved, to ensure hormone levels remain balanced and to check for tumor recurrence.
Conclusion
Hypopituitarism and hyperpituitarism are both conditions that arise from dysfunctions in the pituitary gland, but they manifest in very different ways. Hypopituitarism involves a deficiency in one or more hormones produced by the pituitary gland, which can lead to a range of symptoms, including fatigue, weight loss, growth delays, and reproductive issues. In contrast, hyperpituitarism is characterized by an overproduction of hormones, often due to pituitary adenomas, leading to symptoms such as rapid growth, weight gain, and metabolic disturbances.
Both conditions require accurate diagnosis and tailored treatment approaches to manage hormone imbalances and alleviate symptoms. Treatment for hypopituitarism typically involves lifelong hormone replacement therapy, while hyperpituitarism is often treated through surgery, medication, or radiation to reduce hormone levels. Understanding the differences between these conditions is crucial for effective treatment and long-term management, allowing individuals with pituitary disorders to maintain a better quality of life through proper medical care and monitoring.
In conclusion, while both hypopituitarism and hyperpituitarism stem from issues within the pituitary gland, their effects on the body, symptoms, and treatment options differ significantly. Early diagnosis and appropriate intervention are key to managing these conditions and preventing complications that can arise from hormonal imbalances.
FAQs
What is the main difference between hypopituitarism and hyperpituitarism?
Hypopituitarism involves a deficiency in hormone production by the pituitary gland, while hyperpituitarism involves an overproduction of hormones, usually due to a pituitary adenoma.
Can hypopituitarism and hyperpituitarism be cured?
Hypopituitarism generally requires lifelong hormone replacement therapy as a cure is not usually possible. Hyperpituitarism can sometimes be cured if a pituitary adenoma is surgically removed, but ongoing monitoring is necessary.
How are hypopituitarism and hyperpituitarism diagnosed?
Both conditions are diagnosed through blood tests that measure hormone levels. Imaging tests, such as MRI or CT scans, are often used to identify tumors or structural abnormalities in the pituitary gland.
What are common symptoms of hyperpituitarism?
Symptoms can include rapid growth (in children), enlarged hands and feet (acromegaly), weight gain, high blood pressure, irregular menstrual cycles, and sexual dysfunction.
Can hormone imbalances from these conditions affect fertility?
Yes, both hypopituitarism and hyperpituitarism can affect fertility by disrupting the production of hormones that regulate the reproductive system, such as luteinizing hormone (LH) and follicle-stimulating hormone (FSH).
Related Topics
- All
- Animals
- Diseases
- Health
- Money
- Politics
© 2024 OnYelp.com. All rights reserved. Terms and Conditions | Contact Us | About us