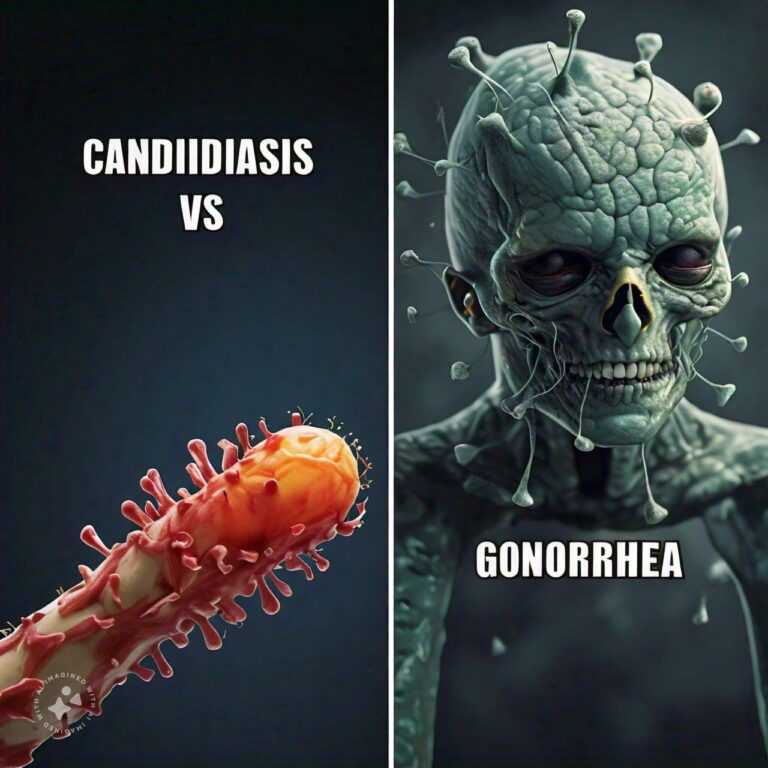
Differences Between Candidiasis and Gonorrhea
Candidiasis and gonorrhea are two distinct infections that can affect various parts of the body, particularly the genital tract. Candidiasis, often referred to as a yeast infection, is caused by an overgrowth of the fungus Candida, particularly Candida albicans, which naturally lives in small amounts in the body. It typically affects warm, moist areas such as the mouth, throat, and vagina. Although candidiasis can be uncomfortable, it is not sexually transmitted and is generally easy to treat with antifungal medications. However, recurrent infections may indicate an underlying health condition, such as diabetes or a weakened immune system.
On the other hand, gonorrhea is a sexually transmitted infection (STI) caused by the bacterium Neisseria gonorrhoeae. It is spread through sexual contact and can infect the genital tract, rectum, and throat. Unlike candidiasis, gonorrhea is a bacterial infection that requires antibiotic treatment. If left untreated, gonorrhea can lead to serious health complications, including infertility and pelvic inflammatory disease (PID) in women, as well as epididymitis in men. While both infections affect the genital region, their causes, transmission methods, and treatments differ significantly, making it important to understand each in detail.
Candidiasis Overview
1. Causes of Candidiasis
Candidiasis is caused by an overgrowth of the Candida species, particularly Candida albicans, a type of yeast that normally resides in various parts of the body, including the mouth, throat, gut, and vagina. Under normal conditions, the body's immune system and beneficial bacteria keep Candida in check. However, certain factors can disrupt this balance, leading to yeast overgrowth and infection.
Common causes of candidiasis include the use of antibiotics, which kill off healthy bacteria that normally control yeast growth, hormonal changes (such as those during pregnancy or from birth control pills), diabetes, and a weakened immune system (due to conditions like HIV/AIDS or chemotherapy). Additionally, wearing tight, non-breathable clothing, poor hygiene, and high sugar intake can create an environment conducive to yeast growth.
2. Symptoms of Candidiasis
The symptoms of candidiasis vary depending on the part of the body affected. Vaginal candidiasis is characterized by itching, burning, redness, and a thick, white discharge that resembles cottage cheese. Women may also experience pain during urination or intercourse. Oral candidiasis, also known as thrush, presents with white patches on the tongue, inner cheeks, and throat, which may be painful or cause difficulty swallowing.
In some cases, candidiasis can affect the skin, leading to red, itchy rashes in areas such as the groin, under the breasts, or between the toes. People with compromised immune systems may develop more serious forms of candidiasis, such as invasive candidiasis, where the infection spreads to the bloodstream and internal organs, potentially becoming life-threatening.
3. Diagnosis of Candidiasis
Diagnosing candidiasis is typically straightforward and based on the symptoms and physical examination of the affected area. For vaginal candidiasis, a healthcare provider may take a sample of the vaginal discharge and examine it under a microscope to confirm the presence of yeast. In cases of oral thrush, a throat swab may be taken to identify the fungal infection.
For skin candidiasis, visual examination is usually sufficient, but in some cases, a small skin scraping may be taken for lab analysis. In cases where invasive candidiasis is suspected, blood cultures or imaging tests may be required to confirm the spread of the infection.
4. Treatment for Candidiasis
Candidiasis is generally easy to treat with antifungal medications. Vaginal yeast infections can be treated with over-the-counter antifungal creams, suppositories, or oral medications like fluconazole. Oral candidiasis is treated with antifungal mouth rinses or lozenges, and in more severe cases, systemic antifungal drugs may be prescribed.
For skin candidiasis, topical antifungal creams and good hygiene practices are usually sufficient. Invasive candidiasis requires immediate medical attention and is treated with intravenous antifungal medications in a hospital setting. Maintaining a healthy immune system and reducing risk factors such as avoiding excessive antibiotic use, improving hygiene, and managing diabetes can help prevent recurring infections.
5. Prevention of Candidiasis
Preventing candidiasis involves maintaining a balance between the body's natural bacteria and yeast. Good hygiene is essential, especially in areas prone to moisture and warmth. Wearing loose-fitting, breathable clothing can help reduce the risk of skin and vaginal yeast infections. Women should avoid scented hygiene products, douches, and harsh soaps that can disrupt the natural pH balance of the vagina.
Managing underlying health conditions, such as controlling blood sugar levels in diabetes, is crucial in preventing candidiasis. Additionally, avoiding unnecessary antibiotic use can help maintain the natural bacterial flora that keeps yeast growth in check. For those prone to recurrent infections, healthcare providers may recommend preventive antifungal treatments.
Gonorrhea Overview
1. Causes of Gonorrhea
Gonorrhea is caused by the bacterium Neisseria gonorrhoeae, which is primarily spread through sexual contact, including vaginal, anal, and oral sex. The infection can affect various parts of the body, most commonly the genital tract, but it can also infect the throat, eyes, and rectum. It is one of the most common sexually transmitted infections globally, particularly among sexually active individuals aged 15 to 24.
Gonorrhea can also be passed from an infected mother to her newborn during childbirth, potentially causing serious eye infections in the baby. Risk factors for contracting gonorrhea include having multiple sexual partners, not using condoms, and having a history of other STIs. Gonorrhea is often contracted alongside other STIs, such as chlamydia.
2. Symptoms of Gonorrhea
Symptoms of gonorrhea typically appear within 2 to 14 days after exposure, though some individuals may not show any symptoms, especially women. In men, symptoms often include painful urination, a white, yellow, or green discharge from the penis, and sometimes swollen or painful testicles. Without treatment, gonorrhea can lead to complications such as epididymitis, which can cause infertility.
In women, symptoms can be less specific and may be mistaken for other infections, such as yeast infections or urinary tract infections (UTIs). These symptoms include painful urination, increased vaginal discharge, and bleeding between periods. If untreated, gonorrhea can spread to the uterus and fallopian tubes, causing pelvic inflammatory disease (PID), which can lead to infertility, chronic pelvic pain, and ectopic pregnancy.
3. Diagnosis of Gonorrhea
Gonorrhea is diagnosed through laboratory testing of samples taken from the affected area, such as the urine, throat, or genital swabs. Nucleic acid amplification tests (NAATs) are the most commonly used diagnostic tool for detecting the presence of Neisseria gonorrhoeae, as they are highly sensitive and accurate.
In some cases, particularly when the infection has spread to other parts of the body, additional tests such as blood cultures or joint fluid analysis may be necessary to diagnose complications. Routine screening is recommended for sexually active individuals, especially those at higher risk of STIs, to detect and treat gonorrhea early.
4. Treatment for Gonorrhea
Gonorrhea is treated with antibiotics, although drug resistance has become a growing concern in recent years. The current CDC-recommended treatment involves a single intramuscular injection of ceftriaxone, combined with oral doxycycline to treat any potential co-infection with chlamydia. It is essential to complete the entire course of antibiotics and to refrain from sexual activity until treatment is finished to avoid reinfection.
Patients are also advised to notify their sexual partners so they can be tested and treated if necessary. Re-infection is common if both partners are not treated. Follow-up testing is often recommended to ensure that the infection has been fully eradicated.
5. Prevention and Management of Gonorrhea
The best way to prevent gonorrhea is through the consistent use of condoms during all forms of sexual activity, including vaginal, anal, and oral sex. Limiting the number of sexual partners and getting regular STI screenings are also effective preventive measures. Open communication with sexual partners about sexual health and STI status is important in reducing the risk of transmission.
For individuals who have been treated for gonorrhea, it is crucial to avoid sexual contact until they and their partners have completed treatment and have been cleared of the infection. Ongoing education and awareness about safe sex practices are vital in reducing the spread of gonorrhea and other STIs.
Differences Between Candidiasis and Gonorrhea
- Cause:
- Candidiasis: Caused by a fungal overgrowth, primarily Candida albicans.
- Gonorrhea: Caused by the bacterium Neisseria gonorrhoeae.
- Transmission:
- Candidiasis: Not sexually transmitted; caused by factors such as antibiotics, hormonal changes, and weakened immunity.
- Gonorrhea: Sexually transmitted infection spread through vaginal, anal, and oral sex.
- Affected Body Areas:
- Candidiasis: Commonly affects the mouth, throat, skin, and vagina.
- Gonorrhea: Affects the genital tract, throat, rectum, and eyes.
- Symptoms in Men:
- Candidiasis: Rarely affects men; when it does, symptoms include itching or redness of the penis.
- Gonorrhea: Symptoms include painful urination, penile discharge, and testicular pain.
- Symptoms in Women:
- Candidiasis: Itching, burning, and thick, white vaginal discharge.
- Gonorrhea: Painful urination, increased vaginal discharge, and bleeding between periods.
- Complications:
- Candidiasis: Rarely causes serious complications, except in immunocompromised individuals.
- Gonorrhea: Can lead to PID, infertility, and epididymitis if untreated.
- Diagnosis:
- Candidiasis: Diagnosed by examining discharge under a microscope or via culture.
- Gonorrhea: Diagnosed using NAATs or bacterial cultures from swabs or urine.
- Treatment:
- Candidiasis: Treated with antifungal medications like fluconazole or topical creams.
- Gonorrhea: Treated with antibiotics, typically ceftriaxone and doxycycline.
- Drug Resistance:
- Candidiasis: Not commonly associated with drug resistance.
- Gonorrhea: Increasingly resistant to antibiotics, requiring more complex treatment.
- Recurrence:
- Candidiasis: Commonly recurs in women, especially with underlying risk factors.
- Gonorrhea: Reinfection is common if sexual partners are not treated.
Conclusion
Candidiasis and gonorrhea are two infections that, while affecting the genital region, differ in almost every aspect, from their causes and symptoms to their treatments and complications. Candidiasis is a common fungal infection that can be easily treated with antifungals, though it may recur, especially in individuals with risk factors like diabetes or antibiotic use. Gonorrhea, on the other hand, is a sexually transmitted bacterial infection that requires prompt treatment with antibiotics to prevent serious long-term complications, such as infertility and pelvic inflammatory disease.
Understanding the differences between candidiasis and gonorrhea is crucial for diagnosis and treatment. While candidiasis is not sexually transmitted and is typically less serious, gonorrhea can lead to significant health risks if left untreated. Practicing safe sex, getting regular screenings, and maintaining good hygiene can help prevent both conditions, promoting better sexual and reproductive health.
FAQs
Related Topics
- All
- Animals
- Diseases
- Health
- Money
- Politics
© 2024 OnYelp.com. All rights reserved. Terms and Conditions | Contact Us | About us