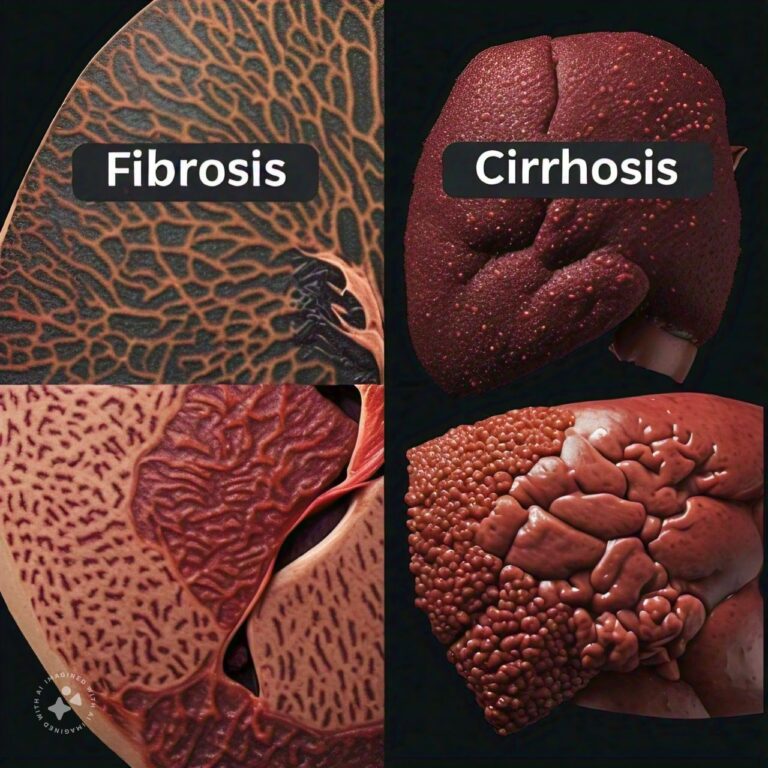
Differences Between Liver Fibrosis and Cirrhosis
Liver fibrosis and cirrhosis are both conditions related to liver damage, but they differ in their severity and impact on liver function. Liver fibrosis refers to the early stages of scarring in the liver, caused by chronic inflammation due to various factors such as alcohol abuse, viral infections, or fatty liver disease. During fibrosis, healthy liver tissue is replaced by scar tissue, but the liver can still function relatively well. If caught early, fibrosis can be reversible, as the liver has an incredible ability to regenerate itself once the underlying cause of the damage is addressed.
Cirrhosis, on the other hand, is the advanced stage of liver scarring. In cirrhosis, the scarring becomes severe, and the liver’s architecture is permanently altered, impairing its ability to function properly. Cirrhosis is often the result of prolonged liver fibrosis that has not been treated, and it is usually irreversible. At this stage, complications such as liver failure, portal hypertension, and liver cancer become more common. While liver fibrosis is often asymptomatic, cirrhosis usually presents with more pronounced symptoms, and treatment is focused on managing the symptoms and preventing further liver damage.
Liver Fibrosis Overview
Liver fibrosis is an early stage of liver damage characterized by the accumulation of scar tissue in the liver. Below are five key aspects of liver fibrosis.
1. What Is Liver Fibrosis?
Liver fibrosis occurs when the liver is repeatedly or continuously damaged, leading to the accumulation of scar tissue. The liver responds to chronic injury by activating specialized cells called hepatic stellate cells, which produce collagen and other extracellular matrix proteins that form scar tissue. This process is the body's natural response to injury, but over time, the excessive accumulation of scar tissue disrupts the normal structure and function of the liver.
- Accumulation of Scar Tissue: Scar tissue forms in response to chronic liver damage.
- Natural Healing Response: The liver creates scar tissue as a protective mechanism, but excessive scarring can impair liver function.
2. Causes of Liver Fibrosis
The most common causes of liver fibrosis include:
- Chronic alcohol abuse: Long-term alcohol consumption can lead to liver inflammation and scarring.
- Viral hepatitis: Infections such as hepatitis B and C are leading causes of chronic liver inflammation and fibrosis.
- Non-alcoholic fatty liver disease (NAFLD): Fat accumulation in the liver, often associated with obesity, can cause inflammation and fibrosis.
- Autoimmune liver diseases: Conditions like autoimmune hepatitis can trigger chronic inflammation and fibrosis.
- Genetic conditions: Diseases such as hemochromatosis (iron overload) and Wilson’s disease (copper buildup) can also lead to liver fibrosis.
- Alcohol Abuse and Viral Hepatitis: Leading causes of chronic liver damage and fibrosis.
- NAFLD and Genetic Conditions: Fatty liver disease and genetic disorders can also contribute to fibrosis.
3. Symptoms of Liver Fibrosis
Liver fibrosis is often asymptomatic, especially in its early stages. As the condition progresses, patients may experience vague symptoms such as:
- Fatigue: Feeling unusually tired or fatigued can be an early sign of liver damage.
- Mild discomfort in the upper abdomen: Some people may experience discomfort or pain in the upper right side of the abdomen, where the liver is located.
- Unexplained weight loss: In some cases, individuals may lose weight without a clear reason.
- Elevated liver enzymes: Liver function tests may reveal elevated liver enzymes, indicating liver damage, even if symptoms are not apparent.
- Asymptomatic in Early Stages: Liver fibrosis may not present noticeable symptoms initially.
- Fatigue and Mild Discomfort: Symptoms can include fatigue and discomfort in the upper abdomen.
4. Diagnosis of Liver Fibrosis
To diagnose liver fibrosis, doctors typically rely on a combination of tests, including:
- Blood tests: Liver function tests, including tests for liver enzymes (ALT, AST), can indicate liver damage. Specialized blood tests like the FibroTest or FibroSure can help estimate the degree of fibrosis.
- Imaging tests: Non-invasive imaging techniques such as FibroScan (transient elastography) and MRI elastography are used to assess liver stiffness, which correlates with the degree of fibrosis.
- Liver biopsy: In some cases, a liver biopsy may be performed to directly assess the extent of fibrosis by examining a small tissue sample under a microscope.
- Blood and Imaging Tests: Common diagnostic tools for assessing liver fibrosis.
- Liver Biopsy: A more invasive test used to confirm the severity of fibrosis.
5. Treatment and Management of Liver Fibrosis
The treatment of liver fibrosis focuses on addressing the underlying cause of liver damage and preventing the progression to cirrhosis. Key treatment strategies include:
- Lifestyle changes: Reducing or eliminating alcohol consumption and adopting a healthy diet can help halt the progression of fibrosis.
- Medications: For viral hepatitis, antiviral medications may help reduce liver inflammation and prevent further fibrosis. For autoimmune hepatitis, immunosuppressive drugs are used.
- Weight loss: In individuals with non-alcoholic fatty liver disease, losing weight can significantly reduce liver inflammation and fibrosis.
- Lifestyle Modifications: Abstaining from alcohol and maintaining a healthy diet are key to managing fibrosis.
- Medications: Antivirals for hepatitis and immunosuppressants for autoimmune diseases can prevent further damage.
Cirrhosis Overview
Cirrhosis is the advanced stage of liver scarring, where the liver's structure and function are severely compromised. Below are five key aspects of cirrhosis.
1. What Is Cirrhosis?
Cirrhosis occurs when the liver undergoes extensive scarring and the healthy tissue is replaced by fibrotic tissue. The scar tissue obstructs blood flow through the liver, causing the liver to shrink and become hardened. Over time, this impairs the liver’s ability to perform its essential functions, including detoxification, metabolism, and bile production. Cirrhosis is considered irreversible, but early diagnosis and treatment can slow its progression and prevent further complications.
- Extensive Liver Scarring: In cirrhosis, scar tissue severely disrupts liver function.
- Impaired Liver Function: The liver becomes unable to perform critical functions such as detoxification and protein synthesis.
2. Causes of Cirrhosis
The most common causes of cirrhosis include:
- Chronic alcohol abuse: Long-term excessive drinking is a leading cause of cirrhosis.
- Chronic viral hepatitis: Hepatitis B and C can cause chronic inflammation that leads to cirrhosis.
- Non-alcoholic steatohepatitis (NASH): A severe form of fatty liver disease that causes inflammation and liver damage.
- Autoimmune diseases: Conditions like primary biliary cirrhosis and autoimmune hepatitis can lead to cirrhosis.
- Genetic disorders: Hemochromatosis and Wilson’s disease can result in cirrhosis if not treated early.
- Alcohol and Viral Hepatitis: Chronic alcohol abuse and hepatitis infections are leading causes.
- Fatty Liver Disease and Autoimmune Conditions: These can also result in cirrhosis.
3. Symptoms of Cirrhosis
As cirrhosis progresses, it can cause more pronounced and serious symptoms, such as:
- Jaundice: Yellowing of the skin and eyes due to the buildup of bilirubin in the blood.
- Ascites: Accumulation of fluid in the abdomen, leading to swelling and discomfort.
- Varices: Enlarged veins, especially in the esophagus and stomach, that can rupture and cause life-threatening bleeding.
- Confusion and fatigue: Liver failure can lead to the buildup of toxins in the brain, causing confusion and fatigue.
- Weight loss and muscle wasting: As the liver's ability to metabolize nutrients declines, weight loss and muscle wasting can occur.
- Severe Symptoms: Jaundice, ascites, and varices are common symptoms of advanced cirrhosis.
- Fatigue and Cognitive Decline: Toxin buildup can cause confusion and fatigue.
4. Diagnosis of Cirrhosis
Cirrhosis is often diagnosed through:
- Blood tests: Liver function tests (LFTs) can indicate severe liver damage. Elevated bilirubin levels, low albumin, and prolonged prothrombin time (PT) are common markers.
- Imaging tests: Ultrasound, CT scans, and MRI are used to visualize the liver and assess the extent of cirrhosis.
- Liver biopsy: A biopsy can confirm cirrhosis by examining the extent of scarring in liver tissue.
- FibroScan: This non-invasive test measures liver stiffness to assess the degree of cirrhosis.
- Blood and Imaging Tests: Liver function tests and imaging help assess the severity of cirrhosis.
- Liver Biopsy: A biopsy provides a definitive diagnosis.
5. Treatment and Management of Cirrhosis
Cirrhosis treatment focuses on managing complications and preventing further liver damage:
- Lifestyle changes: Stopping alcohol consumption is crucial for slowing the progression of cirrhosis.
- Medications: Diuretics can help manage fluid buildup (ascites), and beta-blockers can prevent variceal bleeding.
- Liver transplant: In cases of end-stage liver disease, a liver transplant may be the only option for survival.
- Nutritional support: High-protein and high-calorie diets are recommended to prevent muscle wasting.
- Complication Management: Medications are used to control ascites and prevent variceal bleeding.
- Liver Transplant: A transplant may be required in advanced cases.
Differences Between Liver Fibrosis and Cirrhosis
- Stage of Disease
- Liver Fibrosis: Early stage of liver scarring.
- Cirrhosis: Advanced stage of liver scarring.
- Reversibility
- Liver Fibrosis: Reversible if treated early.
- Cirrhosis: Irreversible in most cases.
- Severity of Symptoms
- Liver Fibrosis: Often asymptomatic.
- Cirrhosis: Causes severe symptoms like jaundice and ascites.
- Liver Function
- Liver Fibrosis: Liver function is still relatively preserved.
- Cirrhosis: Liver function is severely compromised.
- Complications
- Liver Fibrosis: Fewer complications in early stages.
- Cirrhosis: Risk of liver failure, variceal bleeding, and liver cancer.
- Diagnosis
- Liver Fibrosis: Diagnosed through blood tests and imaging.
- Cirrhosis: Diagnosed through blood tests, imaging, and sometimes biopsy.
- Treatment Goals
- Liver Fibrosis: Focuses on reversing damage.
- Cirrhosis: Focuses on managing symptoms and preventing further damage.
- Impact on Life Expectancy
- Liver Fibrosis: Can be reversed, allowing for a normal life expectancy.
- Cirrhosis: Significantly reduces life expectancy if untreated.
- Appearance on Imaging
- Liver Fibrosis: Liver appears mildly stiff on imaging.
- Cirrhosis: Liver appears shrunken and hardened on imaging.
- Liver Transplant
- Liver Fibrosis: Rarely requires transplant.
- Cirrhosis: Liver transplant is often needed in advanced cases.
Conclusion
Liver fibrosis and cirrhosis are conditions on a spectrum of liver damage, with fibrosis representing the early, potentially reversible stage and cirrhosis being the advanced, irreversible stage. While fibrosis may not present noticeable symptoms, it is critical to diagnose and treat it early to prevent progression to cirrhosis, which brings a host of severe complications and a significant reduction in liver function. Treatment strategies for fibrosis focus on addressing the underlying causes, while cirrhosis management aims to control symptoms and slow further liver damage.
Understanding the differences between these two conditions is vital for recognizing the importance of early intervention and long-term liver health management. Both conditions emphasize the need for lifestyle changes, proper medical treatment, and regular monitoring to preserve liver function and improve quality of life.
FAQs
Related Topics
- All
- Animals
- Diseases
- Health
- Money
- Politics
© 2024 OnYelp.com. All rights reserved. Terms and Conditions | Contact Us | About us