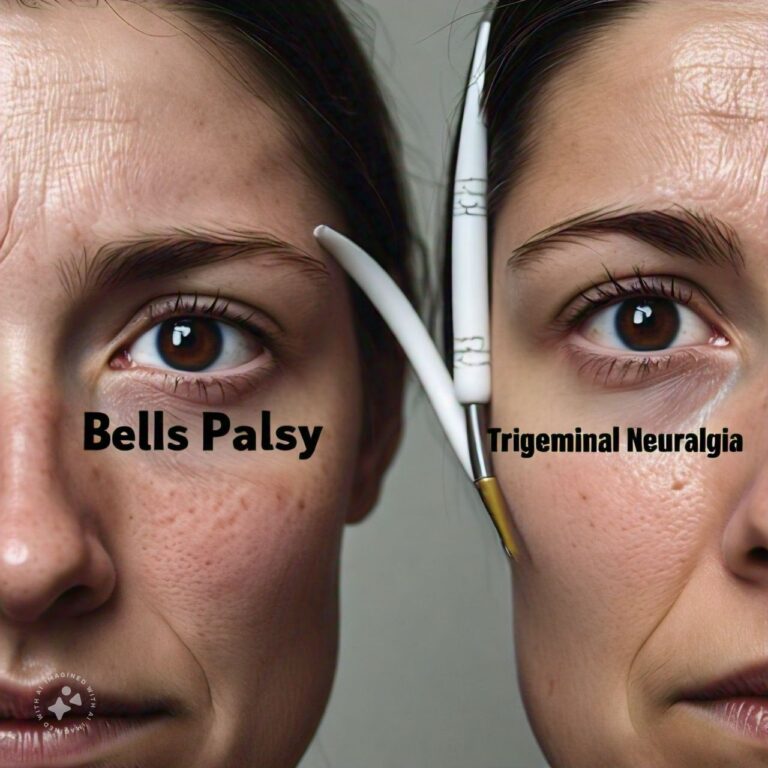
Differences Between Bell's Palsy and Trigeminal Neuralgia
Bell’s Palsy and Trigeminal Neuralgia are two distinct neurological conditions that affect the facial region, though they differ significantly in terms of symptoms, causes, and treatments. Bell’s Palsy primarily involves sudden muscle weakness or paralysis on one side of the face, often leading to a drooping appearance. It is typically linked to inflammation of the facial nerve. On the other hand, Trigeminal Neuralgia is a chronic pain condition that affects the trigeminal nerve, causing sharp, severe facial pain that can be triggered by even the lightest touch.
While both conditions involve facial nerves, the way they manifest and affect a person’s quality of life is very different. Bell’s Palsy often leads to temporary facial paralysis and affects a person’s ability to control facial muscles. Trigeminal Neuralgia, however, is marked by episodes of intense facial pain that can be debilitating. Understanding these conditions is essential for proper diagnosis and treatment, as they both require different approaches.
Bell's Palsy Overview
1. What is Bell's Palsy?
Bell's Palsy is a condition that causes sudden, temporary paralysis or weakness on one side of the face due to inflammation of the seventh cranial nerve, also known as the facial nerve. The facial nerve controls various facial movements, including blinking, smiling, and frowning. The exact cause of Bell's Palsy is still unknown, but it is often linked to viral infections, such as the herpes simplex virus, which may lead to inflammation and swelling of the facial nerve. The condition usually affects one side of the face and can result in an inability to close the eyelid, drooping of the mouth, and difficulty in facial expressions.
2. Symptoms of Bell's Palsy
The onset of Bell's Palsy is sudden, often occurring overnight. Symptoms include facial drooping on one side, loss of ability to close the eyelid, difficulty smiling, a decrease in tear production, and sometimes drooling. Patients may also experience altered taste, ear pain, and increased sensitivity to sound in the affected ear. While the symptoms can be distressing, most cases are temporary, with many patients recovering fully within three to six months. However, in some cases, symptoms can persist or recur.
3. Causes and Risk Factors of Bell's Palsy
Although the precise cause of Bell's Palsy is unknown, viral infections like herpes simplex (responsible for cold sores), varicella-zoster (which causes chickenpox and shingles), and Epstein-Barr (responsible for mononucleosis) are believed to trigger inflammation in the facial nerve. Stress, diabetes, pregnancy, and respiratory infections are considered risk factors that may increase the likelihood of developing Bell's Palsy. People between the ages of 15 and 60 are more commonly affected, although it can occur at any age.
4. Diagnosis of Bell's Palsy
Diagnosing Bell's Palsy involves a physical examination and a review of the patient’s medical history. Doctors will test for the ability to move facial muscles, blink, and make facial expressions. In some cases, imaging tests such as an MRI or CT scan may be performed to rule out other causes, such as a stroke or tumor, which could cause similar symptoms. A diagnosis of Bell's Palsy is typically made when other potential conditions are excluded.
5. Treatment and Recovery for Bell's Palsy
Treatment for Bell's Palsy often includes corticosteroids, such as prednisone, to reduce inflammation and swelling around the facial nerve. Antiviral medications may be prescribed if a viral infection is suspected. Physical therapy, facial exercises, and massage can help to restore muscle tone and prevent permanent muscle stiffness. Most patients recover fully within three to six months, although some may experience lingering effects like facial muscle weakness or spasms. Early treatment improves the chances of a full recovery.
Trigeminal Neuralgia Overview
1. What is Trigeminal Neuralgia?
Trigeminal Neuralgia (TN) is a chronic pain disorder affecting the trigeminal nerve, which is responsible for transmitting sensory information from the face to the brain. The condition is characterized by intense, electric shock-like pain on one side of the face, often triggered by everyday activities like eating, talking, or even brushing the teeth. The pain episodes can last from a few seconds to several minutes, and the condition can significantly impact a person's quality of life due to the unpredictability and severity of the pain.
2. Symptoms of Trigeminal Neuralgia
The hallmark symptom of Trigeminal Neuralgia is sudden, severe facial pain that can be triggered by the lightest of touches, such as a gentle breeze or the brushing of teeth. The pain is often described as sharp, stabbing, or like an electric shock, and it typically occurs on one side of the face. The episodes of pain are usually brief but can recur frequently, leading to prolonged discomfort. Over time, these episodes can become more frequent and more painful.
3. Causes and Risk Factors of Trigeminal Neuralgia
The exact cause of Trigeminal Neuralgia is not always clear, but it is often associated with the compression of the trigeminal nerve by nearby blood vessels. This compression leads to the irritation and malfunction of the nerve, causing the intense pain experienced by sufferers. Trigeminal Neuralgia is more common in older adults, especially those over the age of 50. Multiple sclerosis (MS), a disease that damages the protective covering of nerves, is also a known risk factor for developing Trigeminal Neuralgia.
4. Diagnosis of Trigeminal Neuralgia
Diagnosis of Trigeminal Neuralgia typically begins with a detailed medical history and a physical exam. The doctor will assess the type and location of the pain and look for specific triggers that provoke the symptoms. Imaging tests, such as MRI, may be ordered to determine if a blood vessel or tumor is pressing against the trigeminal nerve, or to identify other conditions like multiple sclerosis that could be contributing to the symptoms.
5. Treatment Options for Trigeminal Neuralgia
Treatment for Trigeminal Neuralgia often involves medications such as anticonvulsants, like carbamazepine, which help to reduce nerve activity and control the pain. Muscle relaxants or antidepressants may also be prescribed in some cases. If medication does not provide adequate relief, surgical options are available. Procedures like microvascular decompression, which relieves pressure on the trigeminal nerve, or gamma knife radiosurgery, which uses targeted radiation, may offer long-term relief. Patients may also find relief through alternative therapies such as acupuncture or nerve stimulation.
Differences Between Bell's Palsy and Trigeminal Neuralgia
- Nature of Condition: Bell's Palsy involves muscle paralysis or weakness, while Trigeminal Neuralgia is characterized by intense facial pain.
- Affected Nerve: Bell's Palsy affects the facial nerve (seventh cranial nerve), while Trigeminal Neuralgia affects the trigeminal nerve (fifth cranial nerve).
- Symptoms: Bell's Palsy causes facial drooping and weakness, whereas Trigeminal Neuralgia causes sharp, stabbing pain.
- Duration of Symptoms: Bell's Palsy usually improves within weeks to months, while Trigeminal Neuralgia can persist for years with fluctuating episodes of pain.
- Pain vs. Paralysis: Bell's Palsy is primarily a motor issue leading to paralysis, while Trigeminal Neuralgia is a sensory issue resulting in pain.
- Triggering Factors: Trigeminal Neuralgia can be triggered by simple actions like eating or speaking, whereas Bell's Palsy has no such triggers.
- Onset: Bell's Palsy typically occurs suddenly and overnight, while Trigeminal Neuralgia pain comes in episodes and can escalate over time.
- Treatment: Bell's Palsy is often treated with steroids and antiviral medications, while Trigeminal Neuralgia requires anticonvulsants or surgical intervention.
- Recovery: Bell's Palsy usually results in a full recovery, whereas Trigeminal Neuralgia often requires ongoing management.
- Associated Conditions: Trigeminal Neuralgia may be associated with multiple sclerosis, while Bell's Palsy is often linked to viral infections.
Conclusion
Both Bell's Palsy and Trigeminal Neuralgia affect the facial region but in very different ways. Bell's Palsy leads to temporary facial paralysis, while Trigeminal Neuralgia is known for intense facial pain. Understanding the differences between the two conditions is essential for accurate diagnosis and treatment. While Bell's Palsy usually resolves with time and appropriate medical intervention, Trigeminal Neuralgia may require more intensive treatment, including medication and possibly surgery. With early and effective treatment, patients with both conditions can manage their symptoms and improve their quality of life.
FAQs
Related Topics
- All
- Animals
- Diseases
- Health
- Money
- Politics
© 2024 OnYelp.com. All rights reserved. Terms and Conditions | Contact Us | About us