Differences Between Panhypopituitarism and Hypopituitarism
Panhypopituitarism and hypopituitarism are both disorders related to the pituitary gland, but they differ in the extent of their effects on hormone production. The pituitary gland, often called the “master gland,” plays a crucial role in regulating various hormonal functions in the body by controlling other glands like the thyroid, adrenal glands, and reproductive organs. When the pituitary gland is damaged or malfunctioning, it can lead to an imbalance in hormone levels, affecting overall health.
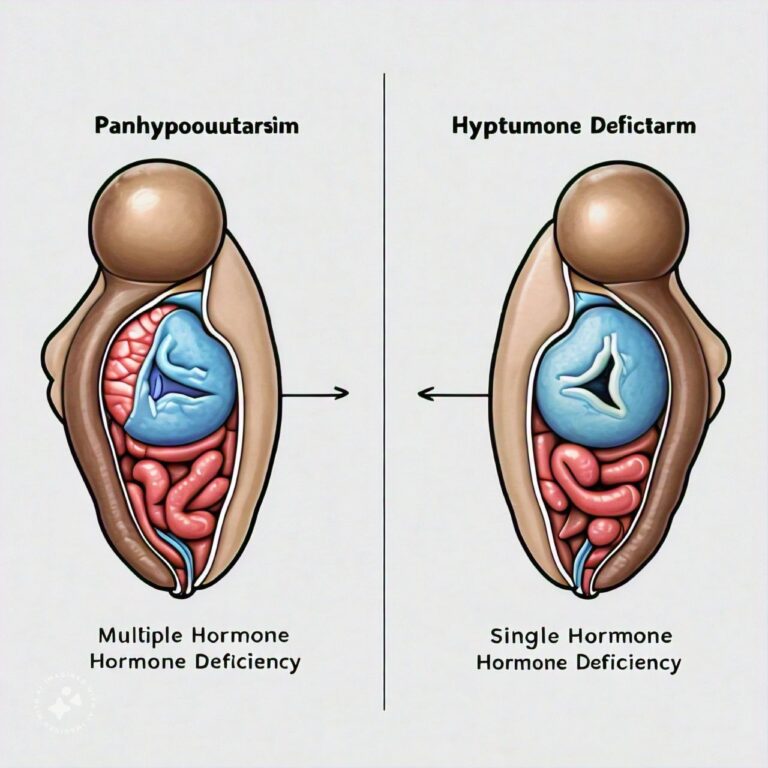
Panhypopituitarism refers to a condition where the pituitary gland fails to produce most or all of its hormones, resulting in widespread hormonal deficiencies. This condition can impact multiple body systems, leading to serious health complications if left untreated. On the other hand, hypopituitarism is a partial deficiency of one or more hormones produced by the pituitary gland. While the symptoms of hypopituitarism can still be significant, they are generally more localized to the specific hormones that are underproduced. Understanding the differences between these two conditions is important for diagnosis and treatment, as the management of each condition may differ based on the hormones involved.
Panhypopituitarism Overview
1. Causes of Panhypopituitarism
Panhypopituitarism occurs when there is a complete or nearly complete failure of the pituitary gland to produce its hormones. This can be caused by a variety of factors, including tumors, traumatic brain injury, infections, radiation treatment, or surgery that damages the pituitary gland. Certain genetic conditions, such as congenital panhypopituitarism, can also result in this condition. Additionally, autoimmune diseases or ischemia (lack of blood flow) can lead to the dysfunction of the gland.
In many cases, panhypopituitarism results from the presence of a pituitary adenoma, a benign tumor that can press on the pituitary gland and impair its ability to function. The extent of hormone loss will depend on the severity of the damage to the gland, but in cases of panhypopituitarism, most or all hormones are affected.
2. Symptoms of Panhypopituitarism
The symptoms of panhypopituitarism can vary depending on the hormones affected but often involve multiple systems in the body due to the widespread hormone deficiencies. Common symptoms include fatigue, weakness, and low blood pressure. Individuals may also experience weight loss, decreased appetite, and sensitivity to cold. Because the condition affects reproductive hormones, patients may experience infertility, decreased libido, or irregular menstruation in women. In more severe cases, panhypopituitarism can cause life-threatening issues such as adrenal insufficiency, where the body cannot properly manage stress or illness.
Symptoms related to thyroid hormone deficiency, such as constipation, dry skin, and hair loss, may also be present. In children, panhypopituitarism can cause delayed growth and development due to a lack of growth hormone. Without treatment, these symptoms can worsen and lead to serious complications.
3. Diagnosis of Panhypopituitarism
Diagnosing panhypopituitarism involves a combination of clinical evaluation, blood tests, and imaging studies. Doctors will typically start with blood tests to measure the levels of various hormones, including cortisol, thyroid hormones, and reproductive hormones. If multiple hormones are found to be deficient, panhypopituitarism is suspected.
Imaging studies, such as an MRI of the brain, are used to assess the structure of the pituitary gland and identify any abnormalities, such as tumors or signs of damage. A stimulation test may also be performed to evaluate the pituitary gland’s ability to release hormones in response to specific triggers. Early diagnosis is essential to prevent further health complications and to begin hormone replacement therapy.
4. Treatment for Panhypopituitarism
The treatment of panhypopituitarism primarily focuses on hormone replacement therapy. Because the pituitary gland is no longer able to produce essential hormones, synthetic versions of these hormones must be administered to the patient. This typically includes cortisol replacement for adrenal insufficiency, thyroid hormone replacement, and sex hormones such as estrogen or testosterone.
In some cases, growth hormone replacement therapy may also be required, especially for children who are still growing. Additionally, desmopressin may be prescribed to manage deficiencies in antidiuretic hormone, which can lead to diabetes insipidus, a condition where the kidneys are unable to conserve water.
Treating the underlying cause of panhypopituitarism, such as surgically removing a tumor or managing an infection, may also be necessary. Regular monitoring and adjustments to hormone replacement therapies are essential to ensure that hormone levels remain balanced.
5. Prevention and Management of Panhypopituitarism
Preventing panhypopituitarism can be difficult, as many of the underlying causes, such as tumors or traumatic brain injury, are not always preventable. However, early detection and treatment of pituitary disorders, such as adenomas, can help reduce the risk of the gland becoming completely dysfunctional.
For those living with panhypopituitarism, regular medical check-ups are necessary to monitor hormone levels and adjust medications as needed. Patients need to be educated about recognizing symptoms of hormonal imbalance and how to manage stress or illness, as these situations can exacerbate the effects of adrenal insufficiency. Proper management can significantly improve quality of life for those with this condition.
Hypopituitarism Overview
1. Causes of Hypopituitarism
Hypopituitarism refers to the partial loss of one or more of the pituitary hormones. The causes of hypopituitarism are similar to those of panhypopituitarism, including tumors, head trauma, radiation therapy, and autoimmune diseases. However, in hypopituitarism, the pituitary gland still retains some functionality and only certain hormones are affected.
In some cases, hypopituitarism may develop gradually due to slow-growing tumors or as a side effect of long-term radiation treatment. In other cases, it may occur suddenly, such as after a head injury or stroke. Hypopituitarism may also be congenital, meaning that a person is born with an underdeveloped or malfunctioning pituitary gland.
2. Symptoms of Hypopituitarism
The symptoms of hypopituitarism vary depending on which hormones are deficient. For example, if the deficiency is in growth hormone, a person may experience fatigue, muscle weakness, and changes in body composition. If the thyroid-stimulating hormone (TSH) is affected, symptoms may include cold intolerance, weight gain, and depression.
When hypopituitarism affects reproductive hormones, women may experience irregular menstrual cycles, infertility, or low libido, while men may experience erectile dysfunction or a decreased sex drive. Unlike panhypopituitarism, the symptoms of hypopituitarism are generally more specific to the hormone that is underproduced, and the overall impact on health may be less severe.
3. Diagnosis of Hypopituitarism
Similar to panhypopituitarism, diagnosing hypopituitarism involves blood tests to measure hormone levels and imaging studies to evaluate the pituitary gland. Blood tests focus on specific hormone deficiencies, such as growth hormone, thyroid hormone, and reproductive hormones.
In addition to hormone testing, doctors may perform stimulation tests to assess the pituitary gland’s ability to release hormones in response to stimuli. MRI scans are commonly used to look for structural abnormalities in the pituitary gland, such as tumors or damage that could be contributing to the hormone deficiency.
4. Treatment for Hypopituitarism
Treatment for hypopituitarism involves replacing the hormones that the pituitary gland is no longer producing. Depending on the hormone deficiency, patients may receive synthetic growth hormone, thyroid hormone, or reproductive hormones like estrogen or testosterone. The goal of treatment is to restore hormone balance and improve symptoms.
In cases where hypopituitarism is caused by a tumor, surgery or radiation therapy may be necessary to remove or reduce the tumor’s size. Patients with hypopituitarism will require lifelong hormone replacement therapy and regular monitoring to ensure that hormone levels remain within a healthy range.
5. Prevention and Management of Hypopituitarism
While not all cases of hypopituitarism can be prevented, early diagnosis and treatment of conditions that affect the pituitary gland can help reduce the risk of hormone deficiencies. For patients who develop hypopituitarism, careful management of hormone replacement therapy is key to maintaining health.
Patients should work closely with their healthcare providers to adjust medications as needed and to monitor for any changes in symptoms. With proper management, many people with hypopituitarism are able to lead normal, healthy lives.
Differences Between Panhypopituitarism and Hypopituitarism
- Extent of Hormone Deficiency:
- Panhypopituitarism: Involves complete or near-complete loss of all pituitary hormones.
- Hypopituitarism: Involves partial loss of one or more pituitary hormones.
- Severity of Symptoms:
- Panhypopituitarism: Symptoms are more severe and widespread due to the loss of multiple hormones.
- Hypopituitarism: Symptoms are generally more localized to specific hormone deficiencies.
- Common Causes:
- Panhypopituitarism: Often caused by large tumors, traumatic injury, or severe infections.
- Hypopituitarism: Can be caused by smaller tumors, gradual damage, or congenital factors.
- Impact on Reproductive Health:
- Panhypopituitarism: More likely to cause infertility or complete loss of libido in both men and women.
- Hypopituitarism: May cause irregular menstruation or erectile dysfunction but often less severe.
- Hormone Replacement Therapy:
- Panhypopituitarism: Requires replacement of multiple hormones.
- Hypopituitarism: May only require replacement of specific hormones, such as thyroid or growth hormone.
- Diagnosis:
- Panhypopituitarism: Blood tests reveal multiple hormone deficiencies.
- Hypopituitarism: Blood tests show a deficiency in one or a few hormones.
- Long-Term Management:
- Panhypopituitarism: More complex, as multiple hormones need to be carefully balanced.
- Hypopituitarism: Treatment is more focused on specific hormone deficiencies.
- Impact on Growth (in children):
- Panhypopituitarism: Causes severe growth delays or failure to thrive due to growth hormone deficiency.
- Hypopituitarism: May cause growth delays if growth hormone is deficient but usually less severe.
- Likelihood of Life-Threatening Complications:
- Panhypopituitarism: Higher risk of serious complications like adrenal crisis.
- Hypopituitarism: Lower risk, but still requires monitoring and management.
- Underlying Cause Treatment:
- Panhypopituitarism: Often requires aggressive treatment of the underlying cause, such as surgery for a large tumor.
- Hypopituitarism: May require less invasive treatments if caused by a small tumor or gradual damage.
Conclusion
Panhypopituitarism and hypopituitarism, while both related to dysfunction of the pituitary gland, differ in the extent of hormone deficiency and the severity of their symptoms. Panhypopituitarism involves a total loss of pituitary function, affecting many hormone systems in the body, while hypopituitarism only impacts one or a few hormones. Both conditions require careful management through hormone replacement therapy, but the complexity of treatment is greater for panhypopituitarism. Early diagnosis and treatment are key to managing both conditions effectively, and patients can enjoy a good quality of life with proper care.
FAQs
Related Topics
- All
- Animals
- Diseases
- Health
- Money
- Politics
© 2024 OnYelp.com. All rights reserved. Terms and Conditions | Contact Us | About us