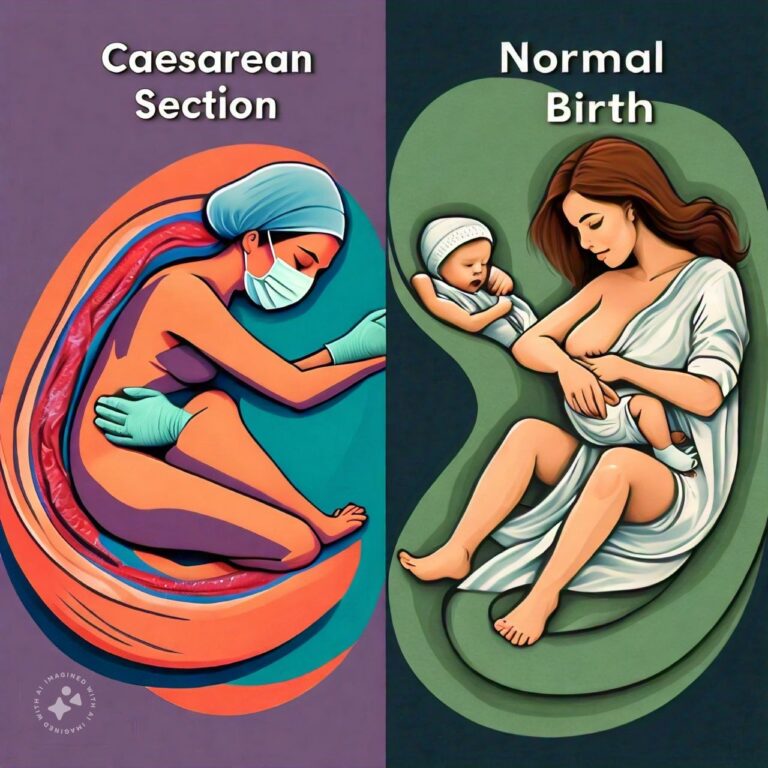
Differences Between Caesarean Section and Normal Birth
Caesarean section and normal birth are two distinct methods of childbirth. While both aim to bring a baby into the world safely, they differ significantly in terms of procedure, recovery time, risks, and overall experience. Caesarean section, commonly referred to as a C-section, is a surgical procedure in which a baby is delivered through incisions made in the mother’s abdomen and uterus. This method is often used when a vaginal delivery poses a risk to the mother or baby, or if complications arise during labor. A C-section may be planned in advance or performed as an emergency procedure if issues develop during labor.
On the other hand, normal birth, also known as vaginal birth, is the natural process in which a baby is delivered through the birth canal. This method of childbirth is generally preferred when there are no complications, as it is associated with a shorter recovery time and fewer surgical risks. While vaginal birth is a natural process, it can sometimes require medical interventions, such as the use of forceps, episiotomy, or pain relief measures like epidurals. Understanding the differences between a C-section and vaginal birth is important for expectant mothers and their healthcare providers to make informed decisions about the best and safest delivery method.
Caesarean Section Overview
A Caesarean section is a surgical procedure used to deliver a baby when vaginal birth is not safe or feasible. Below are five key aspects of C-sections, including why they are performed, the procedure itself, recovery, and potential risks.
1. Reasons for Caesarean Section
A C-section may be planned or performed as an emergency procedure, depending on the circumstances. Common reasons for a planned C-section include previous C-section births, multiple pregnancies (twins or more), placenta previa (where the placenta covers the cervix), or breech presentation (where the baby is positioned feet-first instead of head-first). An emergency C-section may be necessary if complications arise during labor, such as fetal distress, umbilical cord prolapse, or failure of labor to progress.
- Planned C-Section: May be scheduled in advance due to medical conditions or pregnancy complications.
- Emergency C-Section: Performed when issues arise during labor that pose a risk to the mother or baby.
2. The C-Section Procedure
During a C-section, the mother is typically given regional anesthesia (epidural or spinal anesthesia) to numb the lower half of her body, although in some cases, general anesthesia may be used. A horizontal incision is made in the lower abdomen, followed by an incision in the uterus. The baby is then delivered through these incisions, and the surgical team carefully closes the incisions after delivery.
- Anesthesia: Most C-sections are performed with regional anesthesia to keep the mother awake but pain-free.
- Surgical Incision: A horizontal incision is made in the lower abdomen and uterus to deliver the baby.
3. Recovery After a C-Section
Recovery from a C-section typically takes longer than recovery from vaginal birth. The mother may spend several days in the hospital, and it can take 4 to 6 weeks to fully recover. During this time, the mother may experience discomfort or pain at the incision site, and movement may be restricted. Proper wound care is essential to prevent infection, and pain management may be necessary.
- Longer Recovery Time: Recovery from a C-section can take up to 6 weeks.
- Postoperative Care: Proper wound care and pain management are crucial for a smooth recovery.
4. Risks Associated with Caesarean Section
While C-sections are generally safe, they carry certain risks associated with surgery. These include infection, blood loss, and blood clots. There is also a risk of complications in future pregnancies, such as uterine rupture if the mother has a vaginal birth after a C-section (VBAC). Additionally, babies delivered by C-section may have a higher risk of breathing problems initially compared to those born vaginally.
- Surgical Risks: Infection, blood loss, and blood clots are potential risks of C-sections.
- Future Pregnancy Risks: Uterine rupture is a potential risk for women attempting a vaginal birth after a previous C-section.
5. Benefits of a C-Section
Despite the risks, a C-section can be a lifesaving procedure for both mother and baby in certain situations. It allows for the safe delivery of babies when complications like fetal distress, placenta previa, or breech position make vaginal delivery dangerous. It also provides a controlled environment for delivery in high-risk pregnancies.
- Safety for Complicated Pregnancies: A C-section is often the safest option when complications arise during pregnancy or labor.
- Planned Delivery: In cases of planned C-sections, the delivery can be scheduled, allowing for more control over the timing of the birth.
Normal Birth Overview
Normal birth, or vaginal delivery, is the most natural method of childbirth. It involves the baby passing through the birth canal and into the world without surgical intervention. Below are five key aspects of vaginal birth, including the process, benefits, risks, and recovery.
1. The Process of Normal Birth
Vaginal birth occurs in three main stages: labor, delivery of the baby, and delivery of the placenta. During labor, the cervix dilates to allow the baby to pass through the birth canal. The second stage involves pushing and the eventual delivery of the baby, while the third stage involves the delivery of the placenta. Vaginal birth is a natural process, though medical interventions like an epidural for pain relief or an episiotomy (a small cut made to widen the vaginal opening) may be used if necessary.
- Stages of Labor: Labor, delivery of the baby, and delivery of the placenta are the three stages of vaginal birth.
- Medical Interventions: Pain relief methods, such as an epidural, or minor interventions like an episiotomy, may be needed.
2. Recovery After Vaginal Birth
Recovery from vaginal birth is generally quicker than from a C-section. Most mothers are able to go home within 24 to 48 hours after delivery. However, vaginal birth can still cause discomfort, especially if there was tearing or an episiotomy. The perineal area may be sore for several days, and postpartum bleeding (lochia) can last for several weeks.
- Shorter Recovery Time: Most women recover from vaginal birth in a few days, though soreness may last for a few weeks.
- Postpartum Bleeding: Bleeding and discharge can occur for up to six weeks following delivery.
3. Benefits of Vaginal Birth
Vaginal birth is generally associated with fewer complications than a C-section. Mothers tend to experience less blood loss, lower risk of infection, and a faster recovery time. Additionally, babies born vaginally are less likely to experience respiratory problems, as the process of passing through the birth canal helps clear fluid from the baby’s lungs.
- Fewer Complications: Vaginal birth typically involves less blood loss and a lower risk of infection.
- Benefits for the Baby: The baby is less likely to experience respiratory issues compared to those delivered via C-section.
4. Risks of Vaginal Birth
While vaginal birth is generally safe, it does carry some risks, including perineal tearing, prolapsed umbilical cord, and shoulder dystocia (when the baby’s shoulders get stuck during delivery). In some cases, prolonged labor can lead to maternal exhaustion, increasing the likelihood of interventions like the use of forceps or vacuum extraction to assist in the delivery.
- Tearing and Episiotomy: Vaginal birth can result in tearing of the perineum or require an episiotomy.
- Complications During Labor: Prolonged labor or difficult delivery can lead to the need for medical interventions.
5. Pain Relief Options for Vaginal Birth
Women who choose vaginal birth can opt for a variety of pain relief options, ranging from natural methods (such as breathing techniques and water immersion) to medical interventions like epidurals or spinal blocks. The choice of pain relief depends on the mother’s preferences and the circumstances of the delivery.
- Natural Pain Relief: Techniques like breathing exercises or water immersion can help manage labor pain.
- Medical Pain Relief: Epidurals and spinal blocks provide effective pain relief during labor and delivery.
Differences Between Caesarean Section and Normal Birth
- Procedure
- Caesarean Section: Surgical procedure involving incisions in the abdomen and uterus.
- Normal Birth: Natural process involving the baby passing through the birth canal.
- Recovery Time
- Caesarean Section: Longer recovery, typically 4 to 6 weeks.
- Normal Birth: Shorter recovery, usually a few days to a week.
- Anesthesia
- Caesarean Section: Requires regional or general anesthesia.
- Normal Birth: May involve pain relief options like an epidural but does not require anesthesia.
- Hospital Stay
- Caesarean Section: Longer hospital stay (3 to 4 days).
- Normal Birth: Shorter hospital stay (24 to 48 hours).
- Blood Loss
- Caesarean Section: Typically more blood loss due to surgery.
- Normal Birth: Less blood loss compared to a C-section.
- Infection Risk
- Caesarean Section: Higher risk of infection due to the surgical nature of the procedure.
- Normal Birth: Lower risk of infection compared to surgery.
- Pain During Recovery
- Caesarean Section: Pain at the incision site and limited mobility during recovery.
- Normal Birth: Soreness in the vaginal and perineal area, but generally less postoperative pain.
- Future Pregnancies
- Caesarean Section: May increase the risk of complications in future pregnancies (e.g., uterine rupture).
- Normal Birth: Fewer risks associated with future pregnancies.
- Intervention Level
- Caesarean Section: High level of medical intervention.
- Normal Birth: Low to moderate intervention, depending on labor and delivery.
- Impact on the Baby
- Caesarean Section: Higher risk of initial breathing problems.
- Normal Birth: Babies are less likely to have breathing issues.
Conclusion
Both Caesarean section and normal birth are viable methods of bringing a baby into the world, but they differ in terms of procedure, recovery, risks, and impact on both the mother and baby. C-sections are often necessary for complicated pregnancies or emergencies, but they come with longer recovery times and increased surgical risks. Normal birth, when possible, is associated with fewer complications, a quicker recovery, and benefits for both the mother and baby.
Ultimately, the decision between C-section and vaginal birth depends on the mother’s health, pregnancy conditions, and medical advice. It is essential for expectant mothers to discuss their options with healthcare providers to ensure the safest delivery method for both the mother and the baby.
FAQs
Related Topics
- All
- Animals
- Diseases
- Health
- Money
- Politics
© 2024 OnYelp.com. All rights reserved. Terms and Conditions | Contact Us | About us